Introduction
Ovarian vein thrombosis is a rare condition that most commonly occurs during pregnancy and the puerperium. It complicates approximately 0.01 to 0.18% of all pregnancies [1]. Caesarean section has been found to increase the risk of ovarian vein thrombosis. In a prospective study performed in a single centre between 2004 and 2007, the incidence of ovarian vein thrombosis was found to complicate 0.02% of all vaginal deliveries, 0.1% of all deliveries by caesarean section and 0.67% of all caesarean sections for twin pregnancies [2]. Other risk factors include oestrogen-containing treatment, malignancy, pelvic surgery, thrombophilias and certain inflammatory disorders [1].
Thrombosis of the right ovarian vein is more common than the left, with 80-90% of cases occurring on the right side. A possible cause of this predominance to the right side is thought to be the fact that the right ovarian vein is longer with the presence of incompetent valves and absence of retrograde flow [3]. During pregnancy, the enlarged uterus frequently compresses the right ovarian vein at the pelvic brim further contributing to this right sided predominance [1].
Case report
The patient was a 34-year-old Caucasian female who presented to the Accident and Emergency (A&E) department complaining of right iliac fossa (RIF) pain. She had no significant past medical, surgical, or family history. She was previously on the oral contraceptive pill for 16 years. Her weight was 66.6 kilograms. The patient was primiparous, having had a normal vaginal delivery 5 days previously. Labor had been induced following a presentation with recurrent reduced fetal movements at 38+ weeks of gestation. Epidural anesthesia had been administered during labor. She had had a second-degree perineal tear which had been sutured but there had been no antenatal, intrapartum or postpartum complications reported.
Upon presentation at A&E, the patient complained of a three-day history of intermittent RIF pain, which was worse on movement and associated with decreased appetite. A course of co-amoxiclav had been prescribed by her family doctor three days before presentation to A&E in view of a suspicion of urinary tract infection, after which pain progressively improved. She denied any lower urinary tract symptoms, nausea, vomiting, fever or change in bowel habits.
Initial parameters were stable, and she was found to be apyrexial with normal oxygen saturation levels. On general inspection, the patient appeared comfortable and not in pain. Abdominal palpation revealed RIF tenderness with guarding and rebound tenderness but no percussion tenderness. Rovsing's sign, psoas test and renal punches were all negative. There were no signs of deep venous thrombosis in her lower limbs.
Initial laboratory investigations revealed a slightly elevated white blood cell count 11.79 per L (reference range: 4.30 - 11.40 x 109 per L) and C-reactive protein 54.4 mg/L (reference range: 0 - 5 mg/L). Her hemoglobin level was slightly below normal range 11.2 g/dL (reference range: 12.0 - 15.5 g/dL) in keeping with a recent history of vaginal delivery. She was found to have a normal renal profile and normal liver function tests. Urinalysis was not indicative of a urinary tract infection.
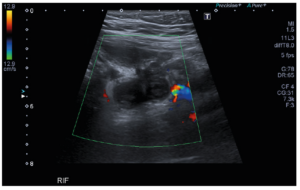
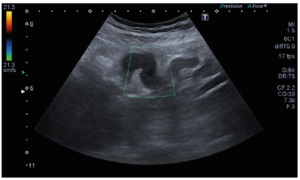
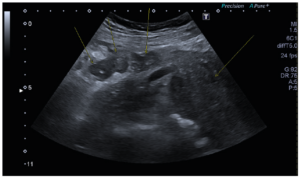
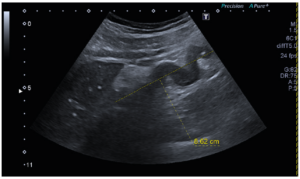
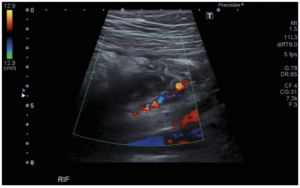
An abdominal ultrasound scan was performed, and the RIF was scanned using a high frequency linear probe and graded compression. In the axial plane, the scan initially showed a cylindrical structure in the RIF with no internal Doppler flow (Figure 1). On scanning in the sagittal plane, this was visualised as a serpiginous non-compressible structure in the RIF (Figure 2). It did not seem to be related to the bowel. No free fluid was seen surrounding this structure. The anatomical shape, size and position of this structure confirmed that it was vascular in nature. The structure was adjacent to the right ovary (Figure 3) and extended cranially towards the right kidney. Its proximal extent could not be fully evaluated. Findings were most in keeping with right ovarian vein thrombosis. The thrombosed ovarian vein was approximately 8.6 cm in length (Figure 4) with surrounding inflammatory changes (Figure 5). The appendix could not be visualised.
Anticoagulation therapy with enoxaparin together with empirical antibiotics were commenced. Following consultation with the haematology team, long term anticoagulation with warfarin or enoxaparin was recommended. The patient responded well to treatment with significant improvement of her pain. The diagnosis of ovarian vein thrombosis within the postpartum period and her admission to hospital placed the patient at risk of pulmonary embolism. Protective factors included her age and normal body mass index. Her vital signs were charted regularly and remained within normal limits. During her admission, the patient denied any symptoms suggestive of pulmonary embolism. She remained in a stable condition and was discharged on the third day following admission on long term enoxaparin therapy and oral antibiotics for a further three days.
The patient was readmitted to the hospital two weeks later with secondary postpartum haemorrhage. A transvaginal ultrasound was suggestive of retained products of conception and an evacuation of retained products was performed. Histological evaluation confirmed scant residual placental tissue with no evidence of malignancy. Patient remained well and was discharged on oral antibiotics for seven days.
The abdominal ultrasound was repeated three weeks after the diagnosis. The previously described serpiginous thrombosed vessel in the RIF demonstrated early signs of recanalization (Figure 6). The inferior vena cava was patent and there was no evidence of thrombus extension. Anti-cardiolipin antibodies, anti-β2 glycoproteins and anti-nuclear antibodies taken six weeks postpartum resulted negative. Nonetheless, the patient was followed-up by the haematology team and a full thrombophilia screen, once off enoxaparin for at least six weeks resulted negative. A magnetic resonance imaging (MRI) of the lower abdomen and pelvis three months following the diagnosis excluded any regional pathologies that might have triggered this event.
Discussion
This case presents a rare condition that is usually not suspected upon presentation. Furthermore, the preferred imaging modality and management pathways are both subjects of debate. Apart from the presentation, diagnosis and initial treatment, this case also describes follow up in terms of investigations and treatment in postpartum ovarian vein thrombosis.
The presentation of ovarian vein thrombosis has been described as a triad of pelvic pain, pyrexia, and a right-sided abdominal mass. Other signs and symptoms such as tachycardia, hypotension, tachypnea, lower quadrant or flank pain, nausea, vomiting, ileus and pyuria have also been described. This condition generally presents within four weeks postpartum, specifically in the first ten days [4].
Imaging modalities used for diagnosis of ovarian vein thrombosis include ultrasonography, computed tomography scan (CT scan) and MRI. On ultrasound, the thrombosed ovarian vein appears as an anechoic or hypoechoic tubular structure extending from the adnexa superiorly and across the iliac vessels with no color-flow or spectral waveform. Ultrasonography may be limited by body habitus and overlying bowel gas [5]. It is also operator dependent. Nevertheless, ultrasound doppler remains the first-line imaging as it is safe, low cost and widely available [1]. On CT scan, the thrombosed ovarian vein appears as a dilated tubular structure containing central low attenuation areas that represent the thrombus. MRI features are similar to CT, but MRI is superior as it allows the differentiation between acute and subacute thrombosis. MRI is the most reliable imaging modality with 100% specificity and sensitivity [5]. In our case, ultrasound was performed at presentation given the availability of expertise in this imaging modality after discussion between two radiologists. CT and MRI scans were not performed at presentation as they would have added little to no clinical benefit in the acute stage. Furthermore, CT involves significant radiation exposure while MRI availability is limited due to high demand.
Complications of ovarian vein thrombosis include sepsis, ovarian failure, and pulmonary embolism. Extension of thrombosis into the renal veins or inferior vena cava can cause ureteral obstruction, hydronephrosis or renal failure, with the latter requiring dialysis in certain cases [6].
Treatment involves antibiotics and anticoagulation. Intravenous broad-spectrum antibiotics should be started upon diagnosis and be continued for at least 48 hours after fever resolution. Longer duration may be required in septic patients. Anticoagulation for 3 to 6 months is recommended for patients with postpartum ovarian vein thrombosis. Anticoagulants which can be used include low-molecular-weight heparin, vitamin K antagonists or direct oral anticoagulants [1]. If the renal vein or inferior vena cava is thrombosed, treatment for pulmonary embolism should be initiated [7].
A recent case report by Ferguson et al. [8] describes a patient diagnosed with ovarian vein thrombosis five days postpartum. The patient was started on enoxaparin, vancomycin and piperacillin-tazobactam. She was then transitioned to apixaban [8]. Another case report by Tsitlakidis et al. [9] describes a patient with right-sided lower abdominal pain, nausea, vomiting and fever who also was diagnosed with postpartum ovarian vein thrombosis. Vancomycin and tazocin were started and later changed to penicillin G and clindamycin following sensitivity results on blood cultures. Anticoagulation with enoxaparin and warfarin overlap was started and patient was discharged on warfarin [9].
Enoxaparin was administered for therapeutic anticoagulation for our patient and the two patients presented by Ferguson et al. [8] and Tsitlakidis et al. [9] during their hospital admission. Long term anticoagulation varied between enoxaparin, apixaban and warfarin. The choice of empirical antibiotics was different. In our case report, the patient was started on intravenous co-amoxiclav. Ferguson et al. and Tsitlakidis et al. both report on a combination of two potent antibiotics as empirical treatment.
When ovarian vein thrombosis is the only site of thrombosis in postpartum patients, investigations for thrombophilia are usually unnecessary [10]. The Royal College of Obstetricians and Gynaecologists recommends that investigations for thrombophilia should only be considered if the results would influence the patient’s future management such as prophylaxis in future pregnancies. The results of thrombophilia testing should not influence the duration and intensity of acute treatment. If investigations for thrombophilia are performed, these should be performed once anticoagulation has been stopped [11].
In conclusion, given the rarity of the condition and its vague symptomatology, a high index of suspicion is required for the diagnosis of ovarian vein thrombosis. There is a broad differential of more common diagnoses for postpartum patients presenting with lower abdominal pain. The choice of imaging modality should be based on the clinical picture and availability of resources and expertise. Prompt diagnosis and treatment with antibiotics and anticoagulants is crucial to prevent life-threatening complications.
Authors’ contributions
MLV: conception and design, analysis and interpretation of the data, drafting of the article, critical revision of the paper, final approval.
KV and HC: critical revision of the article, final approval. TBB and KC: drafting of the article, analysis and interpretation of the data, final approval.
Conflicts of interest
The authors declare having no conflicts of interest.
Ethics statement
The patient in question gave written informed consent for inclusion of her data in this case report.
Funding
None.