Introduction
Violence against women (VAW) is a pressing global issue that poses a number of significant health risks. Although we currently lack precise data regarding the number of women who have been victims of violence, it is a pervasive social problem, with at least one in four women reaching menopause estimated to have experienced violence [1].
Given the impaired neuroendocrine function observed in women who have experienced violence, it is of interest to examine whether VAW can cause immediate or lasting effects after it has occurred [2]. A 2022 systematic review and meta-analysis found that a lifetime history of VAW is associated with increased menopausal symptoms and worse physical, sexual, and psychological health in both peri- and postmenopausal women [3]. Similarly, it has been observed that a history of VAW not only worsens menopausal symptoms, but it also brings forward the age of menarche and increases the risk of premature ovarian insufficiency (POI) [4].
Therefore, it is necessary to investigate the influence of violence on women’s health with a particular focus on its impact on other conditions, such as sexually transmitted infections (STI), menstrual irregularities, reproductive difficulties, and the use of contraceptive methods. Hence, the aim of our study was to analyse whether experiencing any type of VAW increases the risk of gynaecological disorders.
Methods
This cross-sectional study is part of a larger project, which specifically targets premenopausal women who have experienced violence during their lives. As described in the corresponding research paper, VAW is defined as “any act of violence against an individual belonging to the female gender that results in physical, sexual, or psychological harm or suffering for the woman, as well as threats of such acts, coercion, or arbitrary deprivation of liberty, whether this occurs in public or private life”. In addition, economic violence was defined as the control of a woman's ability to obtain economic resources that limits her self-sufficiency [5]. In this observational study, we recruited premenopausal women who had experienced VAW at some point in their lives. Women with pre-existing endocrine or gynaecological diseases before experiencing VAW were excluded. A control group consisted of premenopausal women who attended the same clinic on the same date and who had not suffered from VAW, according to a self-report.
Measures
Clinical data were gathered during the medical interviews, paying special attention to gynaecological disorders such as STI, menstrual irregularities, reproductive difficulties or the use of contraceptive methods. Additionally, the use of medications or toxic substances related to the history of VAW was recorded. Psychological and psychosexual variables were measured through the Patient Health Questionnaire (PHQ-9) and the Generalized Anxiety Disorder (GAD-7) questionnaire.
Information was gathered on independent variables directly related to the type of suffered VAW (economic, psychological, sexual, or physical). Other variables that could potentially influence the history of VAW were also documented, such as socio-demographic factors (age, educational level, employment status, marital status, and residency population size), as well as lifestyle-related control variables (body mass index [BMI], and tobacco or alcohol consumption).
Data analysis
Descriptive statistics, including frequencies and percentages for categorical data and mean values and standard deviations (SDs) for continuous data, were used to summarize key variables and covariates. Multivariate logistic regression analyses were employed to explore the predictors of gynaecological disorders. In cases where it was possible to quantify the effect of VAW on the risk of gynaecological disorders or poorer general or mental health, odds ratios (OR) were calculated for each category using logistic regression. All analyses were conducted using Epidat 3.2 software. Reported P values are two-sided, and a p <0.05 was considered as statistically significant.
Ethical considerations
This study was approved by the FIBAO ethics committee (file number 6hWMS752PFIRMAVHc6wPtZT2+f1x4Y, 7 December 2020). All personal data obtained in this study were confidential and stored and processed following the EU Regulation 2016/679 of the European Parliament. Individuals participating in this study were able to exercise the rights of access, rectification, deletion, limitation of processing, data portability, and opposition established in the regulation mentioned above. All women involved in the study were informed about the study (aims, survey and validated used tools) and gave their informed written consent to participate.
Results
A total of 48 premenopausal women aged 18 to 50 years met eligibility criteria and completed all the surveys. Of the sample, 15 women (31.25%) had experienced VAW at some point in their lives. All participants reported a history of intra-partner violence, and two also reported VAW by a male relative other than their partner. Regarding the type of VAW, 100% of them reported instances of psychological violence, 26.7% economic violence, 40% physical violence, and 33.3% occurrences of sexual violence.
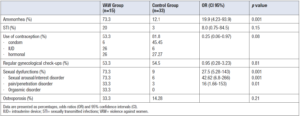
Regarding socio-demographic characteristics, no differences were found between women with or without VAW experience in terms of age and BMI, comorbidities (breast cancer, type 2 diabetes or hypothyroidism), tobacco use or alcohol consumption. However, differences were found in residency population size, education level, relationship status, employment status (Table 1).
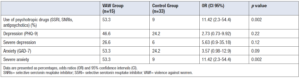
VAW was associated with increased prevalence of amenorrhoea, STI, reproductive difficulties, sexual dysfunctions and less use of contraceptive methods (Table 2). Upon odds ratio calculation a significative higher risk of amenorrhoea (OR 19.9; 95% CI= 4.23-93.9, p <0.001) and sexual dysfunction of any kind (OR 27.5; 95% CI= 5.28-143; p <0.001) were observed in women subject to violence (Table 3).
Discussion
Despite the growing recognition of VAW as a critical issue for women's overall health, a lack of studies still remains that adequately investigate its impact on gynaecological disorders. It is estimated that, for every woman who loses her life due to VAW, more than 400 suffer varying degrees of severe disability. This number rises dramatically when considering other less severe or "silent" disabilities [6,7]. VAW has been associated with increased long-term health risks, spanning a range of issues from chronic pain to severe sexual and psychological disorders [2]. In addition, women who have suffered violence in their lifetime also tend to experience worse menopausal symptoms and increases the risk of POI [7].
In the current study, experiencing any form of lifetime VAW was associated with a 20-fold increase in the risk of presenting amenorrhea and more than a 27-fold increase of sexual dysfunctions (both presented significative higher OR values). When the OR calculation could not be performed (due to the lack of events in the control group) or was not significant, a higher rate of STIs and reproductive difficulties and lower use of contraceptive methods was observed in women subjected to violence. These findings contribute to the limited body of literature on the impact of all types of VAW —both recent and past— on gynaecological disorders.
Of note was the association between having experienced VAW and amenorrhoea. These data coincide with those of a 2008 German survey [8], but to our knowledge, had not been evaluated in an observational study. The fact that amenorrhoea is associated with VAW has important clinical connotations, mainly its repercussions on the health of these women, because if left untreated and perpetuated over time, it could be equated with the consequences of hypoestrogenism in women with sustained central amenorrhoea or POI. In addition, we confirm the significant impairment of the sexual sphere after VAW that has already been described in other studies [9-11]. Dysmenorrhoea, migraines, and generalised pain have also been described [10,11], which did not appear in our series. Regarding pregnancy, although we did not interview any pregnant women in this study, an increased risk of obstetric complications, infections (especially STIs), and miscarriages after VAW has been reported [12].
Another noteworthy aspect was the association between VAW and the consumption of psychotropic drugs and worsening mental health, which is consistent with what has been published in the literature [9,13]. We also observed greater occasional and moderate alcohol consumption among non-maltreated women, which is recognised as social consumption and reveals the lesser relational life of women who have suffered violence. Our results are also consistent with the fact that VAW generally occurs in the family setting, and that it does not require physical or sexual violence to be harmful [4].
Regarding the limitations of our study one can mention mainly the sample size. As already noted in the parent research report and with postmenopausal women [4,5], “this reflects the challenges faced by these women in attending health centres. These difficulties arise both due to personal obstacles faced by the women themselves and because of the administrative barriers imposed by political parties opposed to the concepts related to VAW and to the integral attention of women who are victims of VAW”.
Another limitation comes from the differences observed in the socio-demographic characteristics of the sample. However, in the group of women exposed to VAW there are no features that would suggest that they live in extreme situations that alter their menstrual health: they live in a city of more than 100,000 inhabitants, more than half of them have higher education, own their own home, with the same proportion of being single, married, separated, and their education is mostly egalitarian.
Despite these differences, what this study assesses is the ability of VAW to cause sustained menstrual disorders (amenorrhea), which are not related to these social characteristics, and which can affect women of all social backgrounds.
On the other hand, this association should alert us to the fact that menstrual disorders could add to the signs and symptoms of suspected VAW. It is undoubtedly necessary to detect abused women in any medical consultation to act as early as possible and avoid future complications. Sustained menstrual disorders add to the warning signs that should make us suspect or at least rule out VAW. Other warning signs already described were also present in this study: substance or psychotropic drug abuse, and STIs, as well as some mental disorders (depression, anxiety). Consequently, the protocols for dealing with these situations and recognising the warning signs must be known [14]. Active surveillance is a fundamental pillar, as will be the subsequent comprehensive care of women if there is such involvement. All this supports the need to include in the anamnesis the question of whether the woman suffers or has suffered VAW.
Conclusion
In this cross-sectional study, VAW was found to be associated with higher prevalence of gynaecological disorders such amenorrhoea, sexually transmitted infection, reproductive difficulties, sexual dysfunctions, and less use of contraceptive methods. Experiencing any form of VAW at any point in a ’woman’s life can have a detrimental impact on her overall health, particularly on amenorrhoea and sexual dysfunction. The importance of amenorrhoea is not only because of the lack of menstruation but also because of the long-term repercussions related to hypoestrogenism.
Author contributions
MD: conception of the manuscript, acquisition, analysis and interpretation of data; drafting and revising the article critically for important intellectual content. LMH: conception and design of the study, acquisition of data, drafting and revising the article critically for important intellectual content. IGJ: conception and design of the study, analysis and interpretation of data, drafting and revising the article critically for important intellectual content. NM: conception and design of the study, analysis and interpretation of data, drafting and revising the article critically for important intellectual content.
Author’s agreements
All authors have read and approved the final version of the manuscript, and warrant that the article is the authors’ original work, has not been published previously, is not under consideration for publication elsewhere, and will not be published elsewhere in any format.
Disclosure: This manuscript has been edited and proofread using the trinka tool (www.trika.ai).