Introduction
Life expectancy for women is increasing progressively worldwide. Mean life expectancy for women in the United States is 80 years, while women who are currently 75 years old can expect 12.4 additional years of life [1]. Life expectancy has also increased for Mexican women, to 80 ± 3.82 years [2,3].
Menopause is defined as the final menstrual period (FMP) and is usually confirmed when a woman has had amenorrhea for 12 consecutive months. The mean age at which this occurs in the United States is 51.3 years, ranging between 43.8 and 53.0 years [4-6]. Among women residing in Mexico, menopause occurs at 47.9 years on average [2]. Factors associated with an earlier onset of menopause include: low economic income, low level of education, living more than 2,000 meters above sea level, having a body mass index (BMI) higher than 30 kg/m2, and the lack of physical activity [3-8].
Vasomotor symptoms, commonly described as hot flushes, is the most common symptom experienced by up to 80% of women transiting the menopause and after [9]. A large majority of women rate their vasomotor symptoms as moderate to severe and describe their experience as a sensation of heat with sweating [10,11]. Symptoms persist for a mean of 7 to 10 years, although this seems to depend on the time of onset [12,13].
The impact of vasomotor symptoms in women is related with sleep alterations, fatigue, anxiety, and depression, which can impair the development of daily and work activities [14-17].
The purpose of this study was to design and deploy a survey for peri- and postmenopausal women aged 40 to 65, to determine the prevalence of moderate to severe vasomotor symptoms. Secondarily, data were collected to help understand the economic burden of vasomotor symptoms, in terms of usage of healthcare resources, number of women seeking medical care, and the number of women receiving drug therapy 18]
Methods
Study design
A cross-sectional survey was conducted in a sample of peri- and postmenopausal women living in Mexico, with ages between 40 and 65, who experienced moderate to severe menopause-related vasomotor symptoms. ISN Registration: 2693-MA-3235. This survey corresponds to a sub-analysis of the study published by Todorova et al. [19] (NCT05083884 clinical trial). An active panel was used to contact women, to identify participants as perimenopausal or postmenopausal, and to identify their vasomotor symptoms as moderate or severe.
Study population
Inclusion criteria
Women aged 40 to 65 years were sourced from the national panels of a data collection company, as elucidated in the study by Todorova et al. [19]. Each participant actively consented and successfully completed a screening questionnaire as prerequisites for inclusion in the study.
Exclusion criteria
Women currently in treatment for breast cancer, those treated with estrogen blockers, aromatase inhibitors or gonadotropin releasing hormone (GnRH) agonists / antagonists for cancer or any other activity in the last 12 months [20].
Recorded variables
Patient demographic and clinical characteristics; severity of menopause-related vasomotor symptoms (overall); number of visits to primary care and different types of specialized healthcare professionals (to estimate the economic burden of menopause-related vasomotor symptoms by collecting data from the survey and calculating out-of-pocket expenses); Number of women seeking medical advice and receiving drug treatment, and women’s attitudes towards currently available treatments, as well as their role in the decision-making process.
Used questionnaires
Quality of life
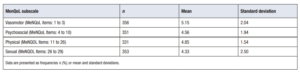
For this study we used the MenQoL in its four specific domains to assess wellbeing (vasomotor; psychosocial; physical; sexual). Each item assesses the impact of one of four domains of menopausal symptoms, as experienced over the last month: vasomotor (items 1–3), psychosocial (items 4–10), physical (items 11–26), and sexual (items 27–29) [21].
Work productivity
Determined using the Work Productivity and Activity Impairment (WPAI) scale in its four domains, assessing work productivity and deterioration in activity over the past week: absenteeism (employed people missing time from work), presenteeism (reduced performance while at work) and employment status change (reduced routine working hours through changing or even losing jobs) [22].
Sleep alterations
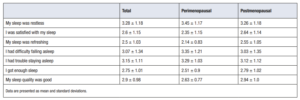
Determined using the PROMIS instrument, which assesses self-reported perceptions on quality of sleep, depth of sleep, and sleep-associated restoration. The 8-item PROMIS Sleep-Related Impairment questionnaire (v. 1.0; 8b) measured self-reported alertness, sleepiness, tiredness, and functional impairments associated with sleep problems during waking hours within the past seven days [23].
Statistical analysis
Statistical analysis was performed with the GraphPad Prism 8.0.1 software (La Jolla, CA, USA). Qualitative variables were expressed as absolute frequencies and percentages, and continuous variables as means and standard deviations, or as medians and interquartile ranges (p75-p25), depending on the normality of data distribution. For all calculations, a p value of < 0.05 was considered as statistically significant.
Results
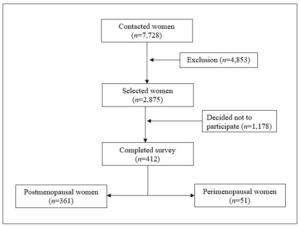
As shown in Figure 1, the panel contacted 7,728 women, of whom only 2,875 met the inclusion criteria, while 1,178 abandoned the study. Of the 1,697 selected women, 412 completed the survey, 12.4% of which were perimenopausal (n=51), and the remaining 87.6% were postmenopausal (n=361). Participant characteristics are described in Table 1.
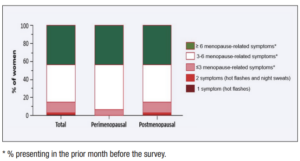
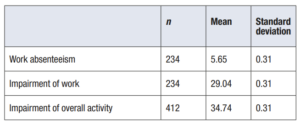
The survey found that the prevalence of moderate to severe vasomotor symptoms was 16.9% (n=61) out of 361 postmenopausal women. Figure 2 shows that most surveyed women presented with more than 3 menopause-associated symptoms in the last month (>80% in both perimenopausal and postmenopausal groups). A 64.8% of the postmenopausal women were actively working (n=234/361). Results of the Work Productivity and Activity Impairment (WPAI) tool indicated that 5.9% of women missed work due to symptoms (3 or more; n=14). A larger percentage (31.6%; n=74) experienced impairment of work productivity. Lastly, the overall impact on impairment of non-work-related activities was determined across the entire studied population (n=412) and vasomotor symptoms were estimated to affect 35.7% of women (n=147) (Table 2).
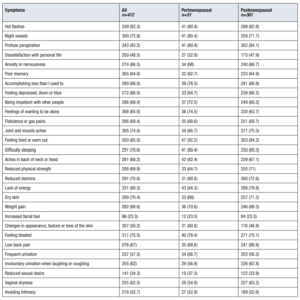
Variables affecting the quality of life of peri- and postmenopausal women were recorded (Table 3a). Results from the MeNQoL quality of life questionnaire in menopausal women showed an overall score of 4.72 ± 2.5 out of 8 (with higher scores indicating a higher negative impact). Table 3b shows the scores for each of the dimensions.
Lastly, sleep quality was determined in peri- and postmenopausal women, showing that 25.9 ± 6.9% of women reported trouble sleeping. Table 4 shows the analysis of each item in the PROMIS scale.
Results showed that out-of-pocket expenses for patients were 1,261 ± 1,136 Mexican pesos over the 3 months prior to the survey. Most surveyed women considered this to be a major expense.
Around 78.4% of the 361 postmenopausal women presenting with moderate to severe vasomotor symptoms sought medical care, and 27.5% had prior medical appointments at least once a month. Of women seeking medical care, 42.1%, 47.4%, and 8.6% visited a specialist, a general practitioner, or an alternative physician, respectively. In the case of women not seeking medical advice, the survey reported that the reason for this was their refusal to take any treatment, especially hormones.
Currently, over half of surveyed women are on some type of treatment: 9.7% on hormone therapy, 3% on bio-identical hormones, 6.6% on non-hormonal therapy, 17.5% on alternative medicine and 34.9% on supplements (i.e. vitamins/calcium).
Discussion
The findings of this survey conducted in the Mexican population show that a relevant proportion of women aged 40 to 65 experience moderate to severe vasomotor symptoms. Prevalence of vasomotor symptoms in our postmenopausal Mexican women reached 17%, which aligns with the prevalence observed in Japanese women (16%), but it is notably inferior to the prevalence observed in European (40%) and US (34%) women [24].
A National Climacteric Survey conducted by the Mexican Association for the Study of Climacteric, focusing on women seeking consultation for symptoms related to the menopausal period, particularly highlighting vasomotor symptoms, revealed a range of prevalent issues. The identified symptoms including physical and mental fatigue (61.0%), irritability (54.2%), depressive mood (54.2%), sleep alterations (53.3%), and joint and muscle discomfort (52.8%) [3].
The most common barriers reported for the use of menopausal hormone therapy (MHT) are fear of increased risk of breast cancer or cardiovascular events, especially in women with a family history of these conditions. In this regard, our results are in line with previously described studies, which also show the presence of these barriers [25,26].
In the present study, women reported a wide range of psychological and physical symptoms in addition to vasomotor events, primarily, feeling tired or worn out (overall: 85% and 84.2% among postmenopausal). Lack of energy was another relevant symptom (reported by 79.8% of postmenopausal women and 80.3% overall), and difficulty sleeping was considered highly troublesome. The SWAN study also reported robust associations between vasomotor symptoms and perceived sleep disorders [27].
Of the surveyed postmenopausal women of our study, 82.8% experienced hot flashes, while 71.7% had night sweats and 84.1% experienced profuse perspiration. A 64.82% of women participants in the study were actively working. Night sweats and hot flashes had a higher impact on daily activities (34.74%) than on work activities (29.04%) [28].
Use of MHT has decreased significantly both in European countries and in the US since the publication of the results of the “Women’s Health Initiative” study, which rose doubts regarding some issues related to the long-term safety of these treatments [29-31]. However, according to the NAMS/IMS guidelines, the optimal safety profile for hormone therapy is observed when initiated in healthy women under the age of 60 or within 10 years of menopausal onset. Consequently, the initiation of hormone therapy in menopausal women aged 60 and older demands a thorough assessment of individual benefits and risks [32-35].
The main strengths of the present study are given by its breadth and the diversity of assessed variables, including the use of validated questionnaires such as the MeNQoL and WPAI.
Conclusions
A proportion of women experience moderate to severe vasomotor symptoms in Mexico. Associated symptoms, such as feeling tired or worn out and sleep-related problems have an impact on the quality of life of women and can impose a significant burden. Given that not all women presenting with moderate to severe vasomotor symptoms actively seek medical attention, telephone panel surveys offer a more robust approximation compared to surveys administered in hospitals or health units which may underestimate the prevalence of vasomotor symptoms. For women currently unable or unwilling to receive MHT, the availability of new treatment options could help improve the management of their vasomotor symptoms.