Introduction
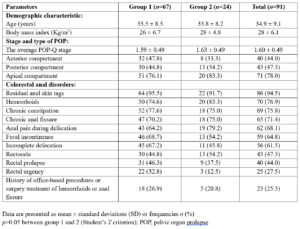
We have been using non-ablative Erbium:yttrium-aluminum-garnet (Er:YAG) laser in our practice since 2018 with good outcomes in women with pelvic floor dysfunction, noticing that the laser treatment also significantly improves their colorectal anal disorders especially in women with pelvic organ prolapses (POP). According to an analysis of data from 72 randomized patient charts, those who seeking our clinic for laser treatment of POP, 93% of them had concomitant colorectal anal disorders such as hemorrhoids, chronic constipation, chronic anal fissure, anal pain, fecal incontinence, incomplete defecation, rectal prolapse, and rectal urgency. The aim of this retrospective study was to analyze the effectiveness of non-ablative erbium laser for the treatment of diverse colorectal anal disorders in women with mild or moderate anatomic POP.
Methods
Study design and patients
This study was a retrospective analysis of data recorded from patient charts at Dr. Pustotina’s Clinic in Moscow, Russia from April 2021 to April 2024 and was conducted in accordance with the Helsinki Declaration. After signing informed consent, we collected data of 91 women aged 25-70 years with diverse colorectal anal disorders and mild or moderate anatomic POP who were treated with the non-invasive 2940 nm Er:YAG laser using the non-ablative SMOOTH® mode. Patients were randomized to Group 1 and 2. Group 1 (n=67) was treated with vaginal, vulvar, and perianal laser irradiation and Group 2 (n=24) was additionally treated with rectal laser irradiation.
Laser treatment
In the 1st step, all patients included in the study received non-ablative Er:YAG treatment for POP, using the ProlapLase® protocol (Fotona, Slovenia). The laser procedure consisted of Er:YAG laser irradiation of the entire vaginal canal with SMOOTH® mode, followed by additional irradiation of the prolapsed anterior and posterior vaginal walls. Depending on the severity of the prolapse, 4-8 passes of laser irradiation were applied. In the 2nd step, the entire vulvar and perianal areas were irradiated after application of transparent water-soluble ultrasound gel to the skin. Patients in Group 2 additionally received rectal irradiation with the non-ablative Er:YAG laser. For the rectal procedure, which we called RectaLase, a PS03 handpiece with a special LA adapter was used. Water-soluble gel was applied to the LA adapter, which was then fully inserted into the rectum. The anterior, posterior, and lateral walls were treated by delivering bursts of four pulses and retracting the handpiece, repeating the laser emission every 5 mm along the distal rectum and anal canal (approximately 4 cm) until reaching the external anal sphincter. We repeated 4 full passes for each wall (a total of 16 longitudinal passes were performed). Standard parameters for mucosa were used: 7 mm spot, 4.5 J/cm2 and 2.0 Hz. In the second step laser energy was decreased to 2.5 J/cm2, and the procedure was repeated along the external anal sphincter (approximately 2 cm).
The procedures were performed in an ambulatory setting, without pre- and post-treatment medications. The treatment time was approximately 30 minutes. Patients received 1 to 5 laser sessions, with 4-6 weeks intervals between consecutive sessions.
Assessment methods
All 91 patients were diagnosed with anterior, posterior and/or apical POP upon vaginal examination. The stage of POP was assessed using the Pelvic Organ Prolapse Quantification (POP-Q) System [1]. Patients with genital prolapse of POP-Q stage more than II were excluded from the study.
Anorectal disorders were diagnosed by patient history and upon vaginal and anorectal examination. They included external and/or internal hemorrhoids, chronic constipation, incomplete anorectal evacuation, chronic anal fissure, anal pain during defecation, fecal incontinence, rectocele, rectal prolapse, and rectal urgency. Patients with anal and colorectal cancer, perianal abscesses, thrombosed hemorrhoids, anal fistulas, condylomas, Crohn disease, malabsorption, and diarrhea were excluded from the study. For the evaluation of colorectal anal symptoms, we modified the Colorectal Anal Distress Inventory - 8 (CRADI-8) questionnaire [2] by including additional parameters (Annex 1). All items were recorded at baseline and after the treatment, using the following format with a response scale from 0 to 4. Symptoms Present = YES, scale of bother: 2 = sometimes, 3 = often, 4 = always. Symptoms Not Present = NO: 0 = not present. A higher score indicates worse symptom bother or a greater impact of symptoms on daily functioning. We also assessed the prevalence of symptoms before and 1-4 months after treatment and recorded adverse events. All collected parameters were included into an anonymized data sheet.
Statistical analysis
Statistical analyses were performed using Microsoft Excel 2000 and Statistica 12 software. The normality of the distribution of variables was determined using the Kolmogorov–Smirnov test. Normally distributed parameters are presented as mean and standard deviations (SD). Normally distributed variables were compared using Student’s T test. Categorical variables were expressed as counts and percentages and compared using Fisher’s exact test. Standardized differences were calculated as means or proportion differences divided by the SD of the difference. The distribution of qualitative indicators in the groups was assessed using the Z-criterion for proportions and the Chi-square test. Changes in qualitative parameters during treatment were evaluated using the McNemar Chi-square test. For all calculations, a p value of < 0.05 was considered as statistically significant.
Results
Ninety-one patients with colorectal anal symptoms and mild or moderate POP underwent combined non-ablative Er:YAG laser treatment (Table 1). In Group 1, patients were treated with vaginal, vulvar, and perianal laser irradiation. They received 1 to 5 laser sessions: 20.9%: 1; 26.9%: 2; 43.3%: 3; 6%: 4; and 3% 5 sessions. Patients of Group 2 were additionally treated with rectal laser irradiation: half of them received 1 and the other half received 2 treatment sessions. The interval between sessions was 4-6 weeks. There were no reported adverse events among the patients. Moisturizing of the vulvar skin, perianal area, and anal canal with transparent water-soluble gel ensure patient comfort and required no additional anesthesia. Laser application to the skin of the entire vulvar and perianal area also allowed excellent aesthetic results, including residual skin tags, irritation and burning. During the rectal laser irradiation, no patient complained except during the treatment of the external anal sphincter area, where mild or moderate pain was observed but did not require any anesthesia.
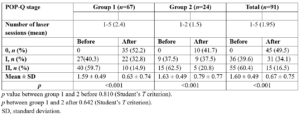
The results of our study demonstrated a significant improvement in both colorectal anal symptoms (Table 2) and (Figure 1) and the stage of POP (Table 3). The overall score of the modified CRADI-14 scale decreased dramatically (p<0.001) from 18.8 ± 4.8 to 6.9 ± 2.4 in Group 1 and from 18.3 ± 5.2 to 4.5 ± 1 scale in Group 2. The patients of the Group 2 with additional treatment by rectal laser, had more benefits on their colorectal anal disorders than Group 1. The improvement in symptoms in Group 2 was significantly greater (p=0.008) than in Group 1 (-13.8 ± 4.7 and -11.9 ± 4.6 scale, respectively), despite Group 2 receiving fewer laser sessions on average (1.5 and 2.4, respectively).
Discussion
Non-ablative erbium laser is one of the newest treatments available for pelvic organ dysfunction [3]. The results of our study corroborate findings from Bizjak-Ogrinc et al. [4], Novakov et al. [5], Alper et al. [6] demonstrating the benefits of non-ablative Er:YAG laser treatment for women with mild and moderate POP. The average POP-Q stage improved significantly from 1.60 ± 0.49 to 0.67 ± 0.75 (p<0.001).
According to our retrospective analysis, 93% of women who applied to our clinic for laser treatment of POP, had concomitant colorectal anal disorders, such as hemorrhoids, chronic constipation, fecal incontinence, chronic anal fissure, rectal prolapse, rectal urgency, and had a history of various office-based procedures or surgery treatment of hemorrhoids or anal fissure. Many of them suffer from rectal bleeding and/or rectal pain during defecation, perianal drainage, anal pruritus, burning and irritation. We are the first to demonstrate the beneficial effect of combining treatment of the vagina, vulva, and perianal area with non-ablative Er:YAG laser in patients with mild and moderate POP and concomitant colorectal anal disorders. Prevalence of colorectal anal symptoms decreased dramatically, and the overall score of the modified CRADI-14 scale changing from 18.8 ± 4.8 to 6.9 ± 2.4 (p<0.001).
The results of our study also demonstrated that additional rectal irradiation with a non-ablative Er:YAG laser along with vaginal, vulvar and perianal treatment enhances the benefits for colorectal anal disorders. The dynamics of symptoms changed more significantly (p=0.008) compared to the patients who received laser treatment without rectal procedure (-13.8 ±4.7 vs -11.9 ± 4.6 scale), despite them having only one or two laser sessions. It is safe to assume that tissue-tightening and neo-angiogenesis effects were achieved in the rectal wall too.
The ultimate result of combining vaginal, vulvar, perianal and rectal erbium SMOOTH® treatments is better pelvic floor support, which helps alleviate or diminish the symptoms of pelvic floor disorders, including POP and colorectal anal symptoms.
Er:YAG laser in SMOOTH mode is safe to use inside the vaginal canal and the rectum, because the laser pulses perform controlled and precise heating of the tissue to depths of several hundred microns, reaching the lamina propria of the mucosa, without ablating or damaging the mucosal surface and underlying structures [7,8]. Moisturizing the vulvar skin, perianal area, and anal canal with transparent ultrasound water-soluble gel before the procedure ensures the comfort of patients, requires no additional anesthesia, and improves even distribution of laser energy. We do not recommend applying lubricants, because they create a protective film which can fully absorb laser energy. The moisturizing gel penetrates the skin, hydrates it, brings it closer to the mucosa, which consists of 90% water, thereby improving the thermal laser diffusion.
Non-ablative SMOOTH Er:YAG is not causing injuries to the mucosa and skin, leaving the surface intact unlike fractional ablative treatment with CO2 or Er:YAG lasers and is reaching comparative depths of penetration, but in a different way – through heat diffusion. Fractional CO2 lasers, even with gradation of treatment invasiveness, perform drilling the microbeams (micro holes) and stimulate the healing of the damaged micro treatment zone producing also the tissue tightening [9,10]. On the contrary, the largest post-marketing clinical trial of vaginal non-ablative Er:YAG laser treatments, which collected data from more than 113,000 patients worldwide, demonstrated the safety of this technology [11]. Moreover, we even recently demonstrated [12] that the intrauterine exposure with a non-ablative Er:YAG laser is safe for the endometrium. Non-ablative thermal diffusion, generated by Er:YAG laser, stimulates synthesis of the new functional glands, neoangiogenesis, and causes restoration of the endometrium.
The present study also confirmed this safety profile for both vaginal and rectal application, as there were no reported adverse events among the 91 treated patients.
This is the first paper presenting the improvement of both colorectal anal symptoms and POP after non-ablative Er:YAG laser treatment. However, this study has the following limitations: there was no control group for comparisons, the follow-up was relatively short and multiple indications were jointly assessed. More clinical trials with higher level of medical evidence are needed to confirm our preliminary results.
Conclusion
Non-ablative Er:YAG laser can be a new option for the treatment for colorectal anal disorders in patients with mild and moderate POP, which are very common among women. We suggest that this method may have beneficial effects in patients with chronic hemorrhoids, whether symptomatic or asymptomatic, anal sphincter dysfunctions, such as incontinence and hypertonicity, rectal prolapse, rectocele and anal fissures. Laser treatment of the vulva and perianal area can also resolve aesthetic problems and dermatitis.
Authors’ contribution
The authors declare the compliance of their authorship according to the international ICMJE criteria.
Consent for publication
Written consent was obtained from the patients for publication of relevant medical information and all accompanying images within the manuscript.
Ethics approval
The approval of the protocol procedure were obtained in accordance with the principles of the Helsinki Convention.
Annex 1.
Modified Colorectal Anal Distress Inventory – 14 item questionnaire
1.Feel you need to strain too hard to have a bowel movement?
2.Feel you have not completely emptied your bowels at the end of a bowel movement?
3.Usually lose stool beyond your control if your stool is well formed?
4.Usually lose stool beyond your control if your stool is loose?
5.Usually lose gas from the rectum beyond your control?
6.Usually have pain when you pass your stool?
7.Experience a strong sense of urgency and have to rush to the bathroom to have a bowel movement?
8.Does part of your bowel ever pass through the rectum and bulge outside during or after a bowel movement?
9.Ever have to push on the vagina or around the rectum to have or complete a bowel movement?
10.Usually have a bulge or something falling out that you can see or feel in your vaginal area?
11.Anal bleeding during defecation.
12.Anal burning.
13.Anal pruritus.
14.Anal irritation.