Introduction
Phyllodes tumor is a fibroepithelial neoplasm with an, incidence that varies from 0.3 to 0.9% of all female breast tumors [1,2]. This tumor presents as a mobile and firm mass, with rapid growth or accelerated growth of a previously stable tumor [3]. From a histological point of view, they are characterized by a foliar architecture, resulting from an enhanced intracanicular growth pattern, elongated spaces similar to slits lined by epithelium and hypercellular stroma, with varying degrees of hyperplasia and atypia [4]. Stromal elements are key components in the differentiation between phyllodes tumors and fibroadenomas, and also in the differentiation between a benign and a malignant tumor [5]. According to the World Health Organization, the classification of this tumor as benign, borderline and malignant is based on some characteristics such as: stromal cellularity, mitotic activity, presence or absence of stromal overgrowth, degree of nuclear atypia of stromal cells and infiltrative or circumscribed margins [6-8].
In addition to the breast, phyllodes tumor can develop in the armpits, vulva and prostate. The vast majority of phyllodes tumors reported in the vulva present as a unilateral, painless mass, located in the labia majora, minora and the posterior margin of the vulva [9,10]. Although it can affect women of all ages, it is most commonly described in women in the perimenopausal age group (42 to 49 years) [11-13].
In total, around 26 cases of phyllodes tumor in the vulva have been reported worldwide, the majority in North America and Europe [14-16]. After reviewing the literature in the PubMed database, without adopting filters, crossing the descriptors [phyllodes tumor] and [vulva], no reports of this type of tumor have been reported in Brazilian patients. Therefore, the present document aims at reporting a case of vulvar phyllodes tumor in a young adult Brazilian woman and its corresponding treatment.
Case report
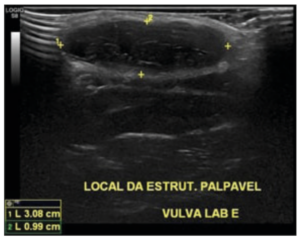
A 23-year-old woman, with no previous comorbidities or family history of neoplasms, attended a gynecological consultation complaining of an uncomfortable vulvar mass, with no precise time of evolution. During the physical breast examination, large, pendulous breasts were observed, with no skin changes, retractions, scars or bulging. On palpation of the right breast, a soft and compressible nodule was identified in the upper lateral quadrant, with a diameter of approximately 1.0 cm. Palpation of the left breast was unremarkable. On genital inspection, a nodule was observed on the left labia majora, without skin changes, hairiness or phlogistic signs. On palpation, a mobile mass was observed, approximately 3.0 cm in diameter, soft, painless and not attached to deep planes. After 30 days, the patient returned to the consultation with the results of breast and transvaginal ultrasound. Breast ultrasound was assigned BIRADs 1 (lesion not visualized where it was previously palpable, suggesting likely reabsorbed simple cyst). The transvaginal ultrasound reported the presence of a subcutaneous hypoechoic nodule of non-specific appearance found in the upper third of the left labia majora, measuring 3.0 x 1.0 x 2.0 cm, without vascularization on Doppler. The probable hypothesis described in the examination report was a thick cyst of the vulva (Figure 1). The proposed medical procedure was excision of the lesion, due to its size and location. However, the patient returned only after 18 months for reevaluation of the condition, with no changes to the physical examination or new complaints. The surgical indication was maintained and, after 10 days, the procedure was performed on an outpatient basis, without complications. The resected surgical material was sent for anatomopathological study. During the surgery, the possibility of tumor removal with a safety margin was not considered, as the phyllodes tumor was not included as a differential diagnosis. The patient had an uncomplicated postoperative period. During the follow-up appointment, she presented no complaints, and upon physical examination, the surgical wound was healed, with no other changes. (Figure 1)
The material that was removed during surgery consisted of a section with a polypoid appearance, measuring 3.5 x 1.5 x 0.8 cm, which was sent for histopathological analysis. The histological examination showed sections of a biphasic, well-circumscribed lesion, with a light fibrous capsule around it, consisting of ducts, some dilated, with a cystic appearance, covered by cuboidal cells without atypia with foci showing hyperplasia, with an extensive foliaceous arrangement, surrounded by bundles of fibroelastic, spindle-shaped cells (Figure 2. A, B, C and D). The histological diagnosis was defined as a histologically benign phyllodes tumor of the mammary-type tissue of the vulvar region, but without margin study. No cellular atypia, mitosis or necrosis were found. The histological picture was compatible with a histologically benign phyllodes tumor of the breast-type tissue of the vulvar region. (Figure 2)
Discussion
Vulvar phyllodes tumor is extremely uncommon, generally benign, painless, and the highest incidence found in the labia majora [17]. It shares microscopic characteristics with phyllodes tumors of the breast, due to the coexistence of specialized glands in the vulva, similar to mammary glands [9].
According to Van der Putte, the first description of the coexistence of fully formed mammary glands in the vulvar labium majora of a 30-year-old patient was in 1872 [18]. However, the first description of a phyllodes tumor in the breast was in 1838 [4,6].
Although rare, there are cases of phyllodes tumors on the vulva reported in several countries such as the United States, Canada, United Kingdom, Switzerland, Spain, Russia, Greece, Turkey, Israel, India, Kuwait, South Africa, Mexico and Colombia [15]. In contrast, after revising the scientific literature and to the best of the knowledge of the authors there have been no reports of vulvar phyllodes tumors among Brazilian women.
Two theories have been proposed to explain the presence of phyllodes tumor in the vulva. The first suggests that it is ectopic breast tissue remaining along the embryonic milk line, which extends from the axilla to the inguinal region [18]. The second theory, more accepted, argues that these are attached and specific structures, present in the anogenital region, with similarities to breast tissue [16,19].
Among the cases reported in the scientific literature, the average age of patients diagnosed with phyllodes tumor in the vulva is 35 years, commonly manifesting between the 3rd and 4th decade of female life [16]. The patient in the present report was diagnosed at the age of 23, was nulliparous, with no gynecological history and no comorbidities. We found only four cases of women younger than this age affected by this tumor in the vulva, one age 17, one 18 and two 20 [9,20,21]. As our patient, in all the cases the histological findings revealed tumoral benignity.
Benign phyllodes tumors of the breast comprise 60 to 75% of all phyllodes tumors and have a risk of recurrence of 17%, which contrasts with malignant tumors, that have a local recurrence risk of 27% and the risk of distant metastasis of 22% [4,22]. Risk factors for recurrence are the histological grade of the tumor, the surgical resection margin and the growth of stromal components [23]. The growth rate of vulvar phyllodes tumors is variable, with some cases showing rapid recent growth, and others, being present without growth for years and discovered as an incidental finding [17].
Histological analysis of the lesion is necessary for the differential diagnosis of vulvar phyllodes tumor and other biphasic tumors, including fibroadenoma, papillary hidradenoma and chondroid syringoma. It may be difficult to distinguish phyllodes tumor from cellular fibroadenomas, as increased stromal cellularity is a characteristic of both [24]. However, phyllodes tumor presents exaggerated intracanalicular stromal growth, with an architecture similar to sheets that project into the lumens and a stroma with greater cellularity, abundant mitoses and cellular atypia [25]. Unlike this, fibroadenomas lack the characteristic leaf architecture and are less cellular and without atypia. Papillary hidradenoma does not have the stromal component present in phyllodes tumor, in addition to the papillary structures being surrounded by a double epithelial layer. The chondroid syringoma has a biphasic nature, but without a sheet-like structure and the presence of cartilaginous components within the myxoid stroma of the syrigoma 14,16,26].
In addition to the histological examination, immunohistochemical tests and genomic evaluation have contributed to the differential diagnosis of phyllodes tumors [14,27]. However, these were not performed in our case. In particular, molecular analysis is recommended in cases without characteristic histopathological and immunophenotypic features.
Considering the rarity of phyllodes tumor in the vulva, it is valuable to highlight its macroscopic presentation, with most studies reporting characteristics of a homogeneous, grayish-white, firm, well-defined lesion with a cystic or solid cut surface. Necrosis and poorly defined margins are rarely observed [17]. These characteristics are similar to the mass observed in the vulvar region of the reported case. In addition, we emphasize that the diameter of the vulvar lesion in the patient's transvaginal ultrasound was 3.0 cm, which is within the limits commonly described in the literature, which can range from 0.7 to 6.6 cm [16]. However, exceptionally, in a Mexican case reported in 2020, researchers described the presence of a vulvar mass on the left labia majora, compatible with a benign phyllodes tumor, measuring approximately 11 cm and weighing 280 g [9].
The current treatment of a vulvar phyllodes tumor is surgical resection with wide margins and surveillance to investigate recurrence of the lesion. Although rare, Heffernan and collaborators have reported recurrence in a lesion classified as benign [26]. The authors attributed this to probable incomplete previous resection. However, after additional resection with clear margins, surgical treatment was considered curative for the case they reported.
In conclusion, phyllodes tumor of the vulva is a rare finding. Among these tumors, the benign type is the most common. Cases of recurrence are uncommon and surgery to resect the mass is not associated with other complications. The histotype of phyllodes tumors and resection margins were the main determinants of local recurrence and distant metastases. Disclosing its clinical manifestations, in addition to macro and microscopic characteristics, is important to carry out the correct diagnosis, as well as provide appropriate treatment.