Introduction
Mycobacterium tuberculosis (TB) infection can give rise to extrapulmonary TB, accounting for approximately 5% of cases in the female genital tract, as a rare form of pelvic inflammatory disease [1,2]. Clique aqui para introduzir texto.Clique aqui para introduzir texto. It profoundly affects reproductive health, contributing to complications such as tubo-ovarian abscesses, subfertility, and pregnancy loss [3,4].Clique aqui para introduzir texto. Due to the insidious nature of female genital TB (FGTB), its rarity and specific epidemiologic contexts, imaging findings may be prone to misinterpretation as indicative of advanced ovarian malignancy or usual bacterial pelvic inflammatory disease [2].Clique aqui para introduzir texto.
Extrapulmonary TB is a secondary manifestation of the primary infection, which is rarely contagious, but it can also occur without a pulmonary infection, due to bacterial dissemination through hematogenous, lymphatic, and direct spread.
FGTB can induce salpingo-peritonitis, giving rise to adhesions, tubo-ovarian masses, that can lead to unilateral or bilateral fallopian tube blockage and subsequent loss of tubal function. Additionally, FGTB has adverse effects on the ovarian function [5]. This case report reveals the intricate intersection of tubo-ovarian abscess formation and the broader implications of genital TB on female reproductive well-being. By exposing this clinical scenario, our aim is to improve comprehension and raise awareness about the complex manifestations of this disease on women's reproductive health.
Case report
A 24-year-old healthy and nulliparous woman from Mozambique, presented with a one-month history of worsening abdominal pain, fever, nausea, vomiting, and persistent diarrhoea. Laboratory results revealed anaemia (Haemoglobin 9.3 g/dL), elevated white blood cell count (20,650 cells/µL with 89.9% neutrophils) and increased inflammatory markers (C Reactive Protein 17.30 mg/L and procalcitonin of 0.33 ng/mL).
Pelvic/abdominal Computed Tomography scan revealed extensive tubo-ovarian abscesses, with the right measuring 10.5 x 6.6 cm and the left 6.5 x 3.5 cm. Multiple loculations with peripheral enhancement suggested inflammatory or infectious aetiology. A possible fistulous tract originating from the distal sigmoid colon extended to the left tubo-ovarian abscess. Additionally, reactive/benign infracentimetric adenomegaly was observed in several left-sided regions (Figure 1). Antibiotic therapy was given during 48 hours with no clinical improvement.
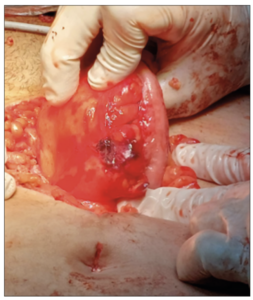
The patient underwent surgery and extensive adhesiolysis. Left colonic fistula (Figure 2), and necrotic changes in the ovaries were observed. A laparoscopic approach was converted to laparotomy for better access and control. The patient underwent total left salpingectomy and proximal right salpingectomy due to challenging access to the distal portion. Additionally, a cystectomy of the right ovarian cyst was performed, and partial excision of the necrotic right ovary was necessary. A colostomy was created to manage the colonic involvement as severe infection and fragile tissues were present.
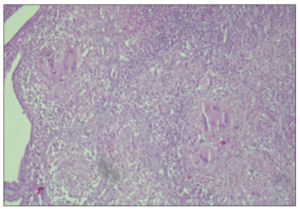
The histopathological report revealed findings suggestive of a chronic granulomatous inflammatory process, raising suspicion for Mycobacterial infection. This aligns with the clinical suspicion of pelvic TB (Figure 3).
Microbiological results of postoperative vaginal swabs indicated the presence of Candida lusitaniae, which was appropriately treated with fluconazole. The patient's Interferon-Gamma Release Assay (IGRA) test returned positive, supporting the suspicion of Mycobacterial infection.
Discussion
Pelvic TB represents a rare yet severe form of extrapulmonary TB affecting reproductive organs. In this case, the clinical presentation, lack of response to antibiotic therapy, surgical findings, and histopathological examination strongly suggested pelvic TB, supported by the histopathological observation of chronic granulomatous inflammatory process indicative of mycobacterial infection.
Diagnosing TB in the pelvic region poses challenges due to the rise of nonspecific symptoms and the need for invasive confirmation procedures. Endoscopic findings, microbiological or molecular testing and histopathological evidence of granulomatous inflammation in gynaecological specimens, are often utilized for diagnosis. Chronic granulomatous inflammation may be a response of the immune system to chronic infections by intracellular microorganisms such as Mycobacterium TB. Recognizing this inflammatory pattern can help clinicians diagnose and appropriately treat these infections [1].
Patients may exhibit symptoms such as abdominal masses, suprapubic tenderness, and fever, that are nonspecific and can overlap with various gynecological conditions such as pelvic inflammatory disease.
When TB affects the female urogenital tract, diagnostic considerations span from acute and chronic bacterial pelvic infections, ectopic pregnancy, endometriosis, various cancers (i.e. ovarian, uterine, or cervical), and even appendicitis. Complications associated with FGTB include vesicovaginal, rectovaginal, tubovesical, urethrocutaneous, tuboperitoneal, and tubo-intestinal fistulae [1,6]. FGTB diagnosis requires confirmation from a combination of tests.
Presently, the World Health Organization recommends three tests for latent TB infection detection: the tuberculin skin test, along with two IGRAs, (QuantiFERON-TB Gold In-Tube and T-SPOT TB), that measure the immune response of T cells to specific antigens associated with Mycobacterium TB infection, aiding valuable knowledge to the diagnosis [6]. If possible, is important to collect biological specimens for the TB culture test. Unfortunately, the TB culture test was not correctly collected, but postoperative IGRA was positive, and the patient was treated accordingly.
In our case, as the patient showed no improvement with antibiotic therapy for pelvic inflammatory disease after 72 hours, the decision to proceed with surgery was prompted by the necessity for a definitive diagnosis and therapeutic intervention.
Concerning the presence of a left colonic fistula, the primary treatment approach is surgical, involving the closure of the fistula, often coupled with salpingectomy. Only one reported case in the literature has documented spontaneous closure [7].Clique aqui para introduzir texto. It is crucial to consider the possibility of tuberculous salpingitis as a potential cause of salpingo-enteric fistula, especially given the increasing number of TB cases in developing countries where the disease is endemic [8,9].Clique aqui para introduzir texto.Clique aqui para introduzir texto.
During surgery, in our case, Fitz-Hugh-Curtis syndrome or acute perihepatitis was observed. This is considered a rare complication of pelvic inflammatory disease, primarily associated with chlamydial or gonococcal infections [10].
Regarding treatment, besides the laparoscopic approach for diagnosis and complication management, multidrug rifamycin-based treatment for 6- or 9-month is adequate [11]. A noteworthy aspect of our case is the co-occurrence of Candida lusitaniae detected by postoperative vaginal swabs. Our patient presented during the postoperative consultation, and swabs were taken due to occasional vaginal pruritus. Although there are no clinical cases in the literature that mention this co-occurrence in pelvic TB, patients with symptomatic lung disease are found to have isolates of non-albicans Candida species. The occurrence of Candida co-infection exhibits a notable female preponderance; some of these patients showed persistence of pulmonary symptoms even after treatment for TB. Screening for both infections seems to be of relevance [12].
Finally, in women with FGTB, infertility impacts 60–80% of cases, and achieving conception remains challenging even following multidrug therapy for TB [12]. In our case, due to bilateral salpingectomy, the patient was referred to an infertility centre, but it seems that this approach should be performed in all patients with FGTB.
Conclusion
This case underscores the importance of a multidisciplinary approach in the management of abdominal TB, particularly when complicated by surgical findings such as extensive adhesions, fistula formation, and ovarian involvement. With a positive IGRA test and histopathological findings, continued investigation is warranted to ensure an accurate diagnosis and appropriate management.
Authorship statement
All authors contributed to patient care, conception of the case report, acquiring and interpreting the data, undertaking the literature review and critically revising the article for important intellectual content.
Funding
None.
Patient consent
Patient consent was obtained for the publication of this case report.