Introduction
Cesarean section (CS) is one of the most common surgical procedures globally, involving delivering of a newborn via surgical incision through the abdominal wall (laparotomy) and then through the uterus (hysterotomy). Worldwide, 21% of births are via CS. This rate has been increasing, with Italy reporting a 31% rate which is above the European average and the WHO's recommended rate of 10-15% [1-3]. Efforts to reduce CS rates where necessary are ongoing, as are efforts to improve safety and outcomes in regions where the procedure is less safe compared to more developed nations. A common goal for patients undergoing a CS and other surgical procedures is to improve recovery. That is why a Swedish study group developed the Enhanced Recovery After Surgery (ERAS) protocols, initially directed to patients who underwent colonic interventions, using a multimodal and multidisciplinary approach based on the best available clinical evidence [4]. This approach has been adapted to many other surgical intervention sites but always includes certain common elements in the entire perioperative period (Box 1). The ERAS Society developed Cesarean delivery protocols (ERAS-CD) between 2017 and 2019, providing maternal and neonatal care recommendations [5-7]. Since then, these protocols have been implemented in many institutions worldwide. In the literature, it is reported that implementing these protocols lead to many benefits, including reduced length of stay (LoS), costs, postoperative complications, and increased patient satisfaction, as observed in many other surgical procedures [8]. A systematic review of the literature up to October 2020 established that ERAS applied to CS significantly reduced postoperative complications, lowered postoperative pain score and opioid use, shortened hospital stays, and potentially reduced hospital costs without compromising readmission rates [9]. Recently, another systematic review published in 2024, that included exclusively studies that used ERAS-CD guidelines reported that this kind of management is associated with decreased LoS and opioid consumption, without negatively impacting readmission rates and overall maternal complications, including surgical site infection and emetic morbidity [10].
The present retrospective study evaluated perioperative clinical outcomes of current management of patients who underwent CS following the introduction of ERAS-CD protocol elements to identify the key factors in the management of these patients in order to achieve early discharge at the Obstetrics and Gynecology Unit of the Santa Chiara Hospital (Pisa, Italy).
Methods
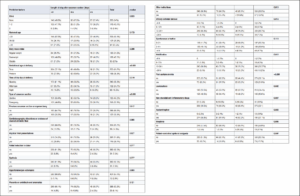
We designed a case-control retrospective study, with cases defined as the patients who had longer stays, and controls as those with an optimal period of stay after the CS of less than three days. Data were collected from the medical records of patients who underwent CS for any indication during 2023 at the Santa Chiara Hospital (Pisa, Italy), considering both emergency and elective procedures, from January 2023 to December 2023. Fifty seven out of the 470 medical records were excluded from our analysis as they were unavailable at the time of data collection. Data variables included demographic, biometric, and obstetric characteristics of patients; surgical indication, time and type of C, the presence of post-partum anemia and postoperative leukocytosis as a possible marker of infection and the type of postoperative analgesic therapy (with or without opioids) and any adverse event during the postoperative period. We chose to assess the time to urinary catheter removal, spontaneous urination, and mobilization as protocol variables, although these elements have not yet been fully implemented due to logistical challenges including staff shortages. For statistical analysis, all variables were categorized into 2-4 groups, and these categorical (qualitative) variables are presented as frequencies and percentages. A univariate analysis was performed using the chi-square test to compare the duration of hospitalization after childbirth with the possible predictive factors. Finally, we performed multivariate linear regression analysis of the factors that emerged as predictive of the LoS in the initial univariate analysis and, therefore, of the failure of early discharge after CS. The significance was set at 0.05 and analyses were conducted using SPSS Version 29.
Results
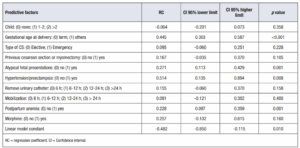
Throughout 2023 (01/2023-12/2023), 470 patients underwent a CS; we collected the data from 413 medical records. Half of the patients were under 35 years of age, 25.9% were between 35 and 39, and 23.5% were 40 or older. Over 50% were nulliparous, and only a small percentage (12 women 2.9%) had more than two children. A 38.3% gave birth prematurely. At delivery, 45.5% of the enrolled women were overweight, and 23% were obese (Table 1). Initial analysis suggested that the number of previous children might have influenced the LoS after cesarean delivery (p=0.023). An association was found between gestational age and LoS, with 72.1% of those discharged in less than three days having full-term pregnancies and 78.7% of those staying five or more days having preterm births (p<0.001). No statistically significant association was found between patient age or body mass index (BMI) and hospitalization duration. Regarding the type of CS, elective or emergency status showed a significant difference, with more days of stay observed among emergent CS (p<0.001). The time of day of the surgery did not significantly impact LoS. A 47.2% (n=195) of patients had undergone elective CS while 218 (52.8%) had undergone emergent surgery. In general, the most common indications in the group of electives CS were previous cesarean or myomectomy (51.8%; 101 cases) and an abnormal fetal presentation (34.9%; 68 cases). In the emergent cesarean section group, the main indications were abnormal cardiotocography (CTG), stained amniotic fluid with 27.0% (59 cases), abnormal fetal presentation 22.0% (48 cases) and failed induction and dystocia, both 14.2% (31 cases each). Globally, the most common indication was a previous CS or myomectomy (30.8%), followed by atypical fetal presentations 28.1% (116 cases) and CTG abnormalities or stained amniotic fluid (14.3%, 59 cases. Less frequent indications included hypertension or preeclampsia (2.9%) and placenta or umbilical cord abnormalities (6.1%). A 13.8% of patients had multiple indications for surgery. There was a significant association between the failure of early discharge and indications such as hypertension or preeclampsia (p=0.003), previous CS or myomectomy (p=0.012), and atypical fetal presentations (p=0.027). Initial analysis of the ERAS-CD protocol elements suggested that the time required to remove the urinary catheter and resume mobilization was significant (both p=0.012), whereas the time to spontaneous urination was not significant (p=0.113). Multimodal postoperative analgesia showed that morphine administration was associated with failure of early discharge (p=0.006). Post-partum anemia, described in 31.9% of patients, was a significant factor for delayed discharge (p<0.001), whereas leukocytosis, reported in 45.6%%, was not. Final multivariate regression analysis indicated that gestational age (p<0.001), hypertension or preeclampsia (p=0.008), atypical fetal presentations (p=0.001), and post-partum anemia (p=0.001) were significant predictors for failure of early discharge (Table 2). Overall, the average LoS for CS patients was 3.3 days. 68.5% of the study population was discharged after 3 post-operative days or fewer. Most procedures were performed under emergency conditions (52.8%). Urinary catheters were classically removed within 12-24 hours, averaging 20.9 hours, and mobilization resumed on average at 21.7 hours.
Discussion
Our preliminary analysis identified a statistically significant association between delayed discharge and gestational age, hypertension or preeclampsia, atypical fetal presentations, and post-partum anemia. However, the time of urinary catheter removal and resumption of mobilization, both key elements of the ERAS protocol not yet implemented at our centre, did not show a statistically significant impact.
This study evaluated perioperative clinical outcomes of current management of patients who underwent CS following the introduction of ERAS-CD protocol elements to identify the key factors in the management of these patients to achieve early discharge. Given the high global rates of CS, optimizing perioperative care is critical to improve clinical outcomes and reduce healthcare costs. The introduction of ERAC (Enhanced Recovery after Cesarean) protocols has shown potential to enhance recovery and promote early discharge.
Despite logistical challenges—such as staff shortages—that hindered the implementation of important ERAS elements like early urinary catheter removal and mobilization, we could still achieve an optimal LoS. This outcome was largely due to the implementation of other ERAS-CD protocol components, including multimodal analgesia and early oral intake. It is important to acknowledge that, given the specific needs of neonatal care, reducing the time of discharge to fewer than two days may not be feasible. Nonetheless, full implementation of the ERAS-CD protocols is highly likely to result in further reductions in LoS, as well as other perioperative benefits, as evidenced in numerous studies.
Even before the ERAS Society guidelines were established, certain elements of ERAS applied to CS had already demonstrated significant benefits. For example, an umbrella review conducted up to October 2014 found that the minimally invasive Joel-Cohen surgical technique, early catheter removal, and postoperative antibiotic prophylaxis significantly reduced LoS after CS—by approximately half to one and a half days. Additionally, the implementation of multi-component ERAS packages showed reductions in LoS ranging from one to four days [11]. These findings suggest that ERAS protocols are both effective and safe. However, due to limitations in the methodological quality of the included studies, more extensive, well-designed, and methodologically rigorous studies are needed to further validate these results [9,11]. The heterogeneity of the studies and the limited number of randomized controlled trials also remain significant limitations [12].
Our findings regarding conditions such as hypertension or preeclampsia align with expectations, given that these conditions are known to cause complications leading to extended hospital stays. Similarly, the association of post-partum anemia with prolonged LoS is unsurprising, as these patients often require additional care. It is also worth noting that the association with preeclampsia may not be fully robust, as only 2.9% of our study population had a diagnosis of hypertensive disorders.
Our results indicate that neither maternal age nor obesity significantly influenced the LoS. However, these findings are limited by the heterogeneity of our study population, which may have obscured potential differences. Comparing more homogeneous groups—such as younger versus older mothers or normoweight versus obese mothers—could reveal variations in LoS. Younger women generally have better overall health and fewer comorbidities, while obesity is often associated with conditions like gestational diabetes and macrosomic fetuses, that could prolong hospitalization. Future studies with stratified or matched cohorts are needed to clarify the impact of these factors on perioperative outcomes.
Preterm deliveries, in contrast, were associated with a longer LoS, primarily due to operational factors. At our institution, mothers of preterm neonates are typically discharged together with their babies once conditions for safe discharge are met, ensuring coordinated care and optimal outcomes. In cases where the neonate requires prolonged medical care, some mothers may opt for an earlier discharge, often for logistical or personal reasons. However, the standard practice remains to keep mothers and their babies together during hospitalization. Further research could explore how discharge practices across institutions influence LoS, particularly in settings where maternal and neonatal discharges are not routinely synchronized.
Our study has several limitations. First, the retrospective design limits our ability to evaluate the true impact of the ERAS-CD protocol. A prospective study with proper randomization—comparing patients managed with and without ERAS-CD protocols—would be essential to eliminate confounding factors and provide a more robust assessment. Second, this manuscript primarily compares differences in patient characteristics rather than offering a comprehensive evaluation of the ERAS-CD protocol, potentially diluting the focus on the protocol itself. Future studies should distinguish between protocol-driven and patient-driven outcomes to better evaluate the protocol’s effectiveness. Lastly, the heterogeneity of our population and the lack of stratification between uncomplicated and complicated pregnancies, combined with the absence of randomization, may introduce judgment bias and affect the reliability of our conclusions. These constraints underscore the need for further research to refine our understanding and optimize ERAS protocol implementation across all stages of the perioperative period.
In conclusion, it is plausible to speculate that the introduction of ERAS components in CS clinical paths should be complete in order to attain major benefits and general postoperative enhanced outcomes as well as faster discharge for patients.