Introduction
A progressive decline in anthropometric characteristics begins in the third decade of life, including bone mass, muscle mass and balance that increases with each subsequent decade [1]. This age-related bone and muscle loss is associated with weakness that significantly increases the risk of physical inactivity, functional limitations, and eventually, falls and bone fractures [2].
Falls in older adults are a common concern among public healthcare professionals and managers. Almost one out of three elder individuals living in nursing homes experience each year at least one fall [3]. This figure rises to one out of two for those aged 80 and over. Falls are also recognized as a major risk factor for osteoporotic fractures [4,5].
There are multiple factors related to falls, many of which are intrinsically linked to the aging process. Changes in sleep patterns are a physiological consequence of aging, as well as a factor involved in the increased risk of falls, with reported rates of non-restorative sleep ranging from 36% to 69% [6,7]. Sleep interruption is the most reported complaint, characterized by frequent awakenings of varying duration [8].
A robust evidence suggests the relation between short sleep duration and the risk of falling in the elderly [9,10], where poor sleep quality interrupts physiological processes leading to daytime drowsiness, decreased attention, impaired cognitive function and reduced psychomotor functioning. This sum of factors contributes to the increased risk of falls observed among older people [11].
In particular, an association between gait difficulties and poor sleeping patterns has been identified, suggesting that the reduction of sleep quality and the related increased gait impairment are good predictors of falls in mid-aged and older women. However, the use of more than one tool for the analysis of physical performance should be considered [12].
Given the relevance and incidence rates of these conditions, the present study was designed with the aim to assess the relationship between sleep quality and physical performance tests as a predictor of falls and fractures among an elder population.
Methods
This cross-sectional study records data from the initial phase of a longitudinal project aimed to develop a fracture risk protocol for frail elderly people to be implemented in healthcare units in the city of Curitiba, Brazil.
Sample
A total of 94 subjects with a mean age of 68.6 ± 6.7 years were included in this study (30 male and 64 females). The sample was divided according to the result of the Pittsburgh Sleep Quality questionnaire as normal (NSQ, n=50) and poor sleep quality (PSQ, n=44), with scores ranging from 0-4 (NSQ) as normal and 5 or more (PSQ) as poor. Socio-economic variables from all participants were recorded, such as partner status, place of residence, work environment, exercise routine and number of children. In addition, anthropometric and clinical variables such as body mass index (BMI), history of diseases and comorbidities such as hypertension, thyroid disease, dyslipidemia, tobacco consumption habit, use of psychotropic drugs, antidepressants, benzodiazepines, melatonin, herbal medicine and menopausal hormone therapy were collected.
Physical function and anthropometric characteristics
Dual-energy X-ray absorptiometry (DXA – Hologic Horizon A, Newark, Delaware USA) was used to assess: total lean mass (TLM), appendicular skeletal mass (according to the European Working Group on Sarcopenia protocol (ASM/H²), and bone mineral density (BMD) of the femoral neck (FBMD) and lumbar spine (LBMD) areas. Physical performance was assessed through handgrip strength (HGS) with a 2 kg precision manual dynamometer Jamar (Sammons Preston Leicestershire, UK). Three attempts were made with the dominant hand, where the highest value was used to classify strength. Gait speed (GST) was assessed through the 4-meter protocol.
Questionnaires
The Pittsburgh Sleep Quality Index (PSQI) in its Portuguese language (Brazil) versions was used to evaluate sleep quality. The PSQI [13] assesses the subjective quality of sleep, sleep duration, sleep efficiency, sleep disturbances, use of hypnotics and diurnal dysfunction. As described above and for the purpose of this study, individuals who scored higher than 5 were defined as bad sleepers or have poor sleep quality, and those who scored less than as good sleepers or have normal sleep quality. In addition, and although not used in the study, the specific analysis of the scores considers that a score under 5 suggests no serious sleep problems but a score from 5 to 7 is an indication to consider starting medical treatment; a score from 8 to 14 requires care and medical treatment and a score from 14 to 21 suggests a severe sleep problem. Questions 10 A (absence or presence of snoring), 10 B (absence or presence of respiratory apneas) and 10 C (absence or presence of leg spasms while sleeping) were categorized as negative score 0 and positive when scored ≥ 1.
Statistical analysis
All statistical analyses were performed using the Statistical Package for the Social Sciences software (version 25.0 - SPSS Inc., Chicago, USA). Results are expressed as frequencies and percentages and for quantitative variables results are expressed as mean and standard deviations. Measures of central tendency and distribution were used to describe the groups and to test for homoscedasticity. The Shapiro-Wilk test and the Kolmogorov-Smirnov test were used to check normality of data distribution. Either the T -test or the Mann-Whitney U test were used to analyze the continuous variables, according to the homogeneity of the variance measured with the Bartlett test. Chi-square test was used to compare qualitative variables. For all calculations a p value of < 0.05 was considered as statistically significant.
Results
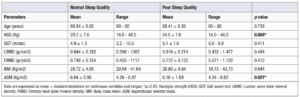
A descriptive analysis of the variables was performed for the total group of 94 participants, who were subsequently divided into 2 groups according to the classification of sleep quality. Clinical and anthropometrical characteristics are given in Tables 1 and 2. Body component and performance tests and descriptive analyses of 94 subjects were divided into two groups: Normal sleep quality (NSQ, n=50) and PSQ (PSQ, n=44).
(Table 1)
Up to 65.9% of the participants were overweight (BMI 27.1 Kg/m2 to 30 Kg/m2). FBMD and LBMD was used to verify bone quality, but we didn’t find statistical difference between groups for these variables. For physical performance we used HGS that was significantly lower in the PSQ group (p =0.004) as well as lower ASM. Although they did not show statistical significance, most of the other analyzed parameters tended to be lower for the PSQ group.
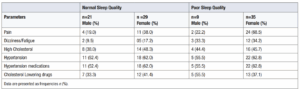
(Table 2)
For both groups, pain was the most reported cause of daily discomfort, followed by dizziness and fatigue. However, for the PSQ group, pain was found in 68.5% of women. Hypertension was the most common condition recorded within the health history, followed by hypercholesterolemia and orthopedic disfunctions, and their respective pharmacological treatments were the mostly used. Furthermore, 15 of the 44 participants in the PSQ group reported use of polypharmacy (4 or more medications). Pain presented in a higher rate in the PSQ group as compared to the NSQ group.
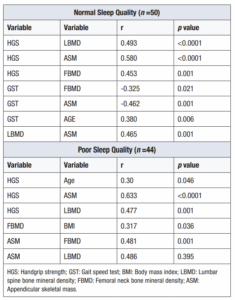
Table 3 (Table 3) shows the variables that directly influenced the components of physical performance and body composition, and their significant association and correlation between the compared groups.
The NSQ group presented moderate and significant correlation between HGS and LBMD and with ASM, while GST showed significant correlation with FBMD, whereas ASM demonstrated significant correlation with FBMD and LBMD. The influence of variables showed HGS with the higher scores on ASM (33%) and LBMD (24%), while GST presented influence on FBMD (10%). As for the influence of muscle mass on bones, ASM showed significant influence on LBMD (21%). PSQ group variables showed that ASM presented influence of (40%, p =0.000) and (25.8%, p =0.000) with HGS and FBMD, respectively, and HGS also presented influence on LBMD. GST presented low influence on bone and muscle variables.
Discussion
The present study examined the intricate relationship between sleep quality, body performance (physical function) and the risk of fractures among older adults. Recent evidence suggests that sleep quality may play a pivotal role in regulating bone health, falls, and fractures. Short or excessive sleep duration, daytime naps, and late sleep can have detrimental effects on bone health [14].
Growing evidence strongly suggests a close relationship between the risk of falls and physical function in older adults, making a clear recommendation to incorporate a more comprehensive evaluation that encompasses muscle strength, balance and gait in the treatment of these patients [15]. A recent study on sarcopenia supports its multifactorial cause and the complexity of its management [16]. In this scenario, not only low muscle mass levels or increase in its loss constitutes an isolated problem for the risk of falls. Similarly, our data shows that 35 of the 44 participants who presented poor sleep quality were overweight, and that this condition is associated with poor levels of muscle mass. We also noticed that the process of losing muscle mass while gradually increasing fatty tissue directly affects performance in the elderly, mainly in those with greater clinical and functional vulnerability. Although most variables did not show significant differences between the groups, the HGS variable for physical performance and the ASM variable for muscle quality showed lower values for the PSQ group and a significant statistical difference.
The aging process often entails a significant decline in sleep quality among individuals classified as frail [17]. A population-based nationwide survey involving 12,759 respondents, aged 50 and older, found that up to 17% experienced falls within the previous 2 years. In the present study we observed that the participants who had nighttime sleep duration of ≤ 5 hours were more likely to report falls than those who had nighttime sleep duration ≥ 6 hours; conversely, there was no association between nighttime sleep duration of > 8 hours and falls. In addition, participants having sleep disturbances for 1–2 days, or 3–4 days, and 5–7 days per week were also more likely to report falls than those who had no sleep disruptions [18]. Other studies have found similar patterns, demonstrating that short sleep duration is also associated with frailty in older people [19,20].
In the present study, we explored sleep profile in association with performance variables, bone quality, physical performance and muscle mass. Despite the statistical significance, age showed a low correlation for both groups in the correlation with the physical tests, which may be related to the similarity of the average age between both groups.
Those relationships were observed in the NSQ group, with higher values in the performance tests corresponding to better outcomes (BMD and muscle mass), where HGS exhibited moderate and significant correlation with LBMD and ASM, while GST displayed a significant correlation with FBMD. Our data agrees with the findings of Ochs-Balcom et al, who demonstrated that short sleep was related to low bone mass density and osteoporosis. In their study involving 11,084 women between 50 and 79 years of age, approximately 10% of the sample slept 5 hours or less, and this group of participants exhibited lower BMD values compared to those women who slept 7 hours or more per night [19]. All these evidences highlight the importance of monitoring and treating sleep disorders and its associated causes in order to reduce the risk of falls and fractures in the elderly.
In the present study, the primary association found within the PSQ group was GST, with moderate and inverse correlation with age, while ASM exhibited correlations with HGS and FBMD (0.633, p <0.0001; and 0.481, p=0.013; respectively). Our findings are similar to a study involving 1,865 individuals, which demonstrated that sleep patterns were associated with BMD and the risk of osteoporosis, and that a healthy sleep is essential for maintaining bone health [15]. In addition, a survey assessing the association of pain, sleep quality and falls, showed significant correlation between sleep disturbances and falls, where 13.56% of those falls resulted in injuries and an increased the risk of fall recurrences. These findings highlight the evidence that pain may be the cause of the main changes associated with poor sleep quality and subsequent falls among elders [21]. Our records suggest that 43.6% of the participants in PSQ group reported pain as the main complaint and common symptom during activities of daily living, followed by dizziness and fatigue with 23% each. However, in this group, 68.5% of women reported pain compared to 22.2% of men. It is believed that women in this age group are more sensitive to pain because they have many associated diseases and report pain more easily than men.
Regarding the influence between variables, in the NSQ group, HGS exerted a greater influence on ASM (33%) and LBMD (22.7%), while GST influenced FBMD (10%). In the PSQ group, the primary significant influences were ASM (40%) on HGS, and ASM (25.8%) on FBMD. GST, considered in the literature an important predictor of falls, presented the lowest value in the PSQ group in comparison to the NSQ group. The relationship between sleep pattern and BMD was also shown in a study involving 169 older adults (71.9 years, 85.5% female) hospitalized due to osteoporotic fractures. Most patients exhibited poor sleep pattern, and the study concluded that this was significantly related to reduced BMD when compared to those who reported healthy sleep [14].
A limitation in our study is that we only evaluated self-reported sleep quality and did not analyze other associated symptoms or its primary causes. We must consider that poor sleep may be associated with other problems linked with aging itself, a condition that makes it difficult to directly be associated with physical performance or a greater isolated risk of falls. This scenario is reported in a study that investigated short and long sleep duration and the increased risk of recurrent falls, where the authors found no statistically significant results despite the fact that short sleep duration was associated with a modest increase in fractures [20]. These findings suggest that more longitudinal studies and a larger sample should be conducted on the relationship between sleep quality and falls and fractures.
The complexity of the relationship between sleep quality and risk of falls is further demonstrated in a study with institutionalized elderly people that were reportedly affected not only by insomnia but to the medications related to this condition and the subsequent risk of falls. The authors concluded that non-pharmacological approaches and better supervision can reduce this scenario [22]. Similarly, in our study we found that 59.5% of the participants in the PSQ group were under medication for hypertension, and that 32.9% of them simultaneously took 4 medications or more, demonstrating that not only the pathology itself, but the pharmacological treatment behind them, can have a significant influence on sleep quality and its consequences. A cross-sectional study that assessed 178 elderly residents in nursing homes found that having low muscle strength indicates poor sleep quality which, in turn, influences low physical function, nutritional quality and depression. Thus, sleep quality was a consequence of these changes, where the primary causes should be the objective of treatment [23].
Conclusion
The control and management of the variables that affect the risk of falls is essential to prevent fractures and their subsequent comorbidities in the elderly population. Our study aimed to evaluate sleep quality in a group of frail older people, linking the results to their performance and bone quality. Our findings show that poor sleep appears to impair gait speed, strength, lean mass and BMD, increasing both the risk of falls and fractures. However, it cannot be excluded that sleep disorders and falls are a consequence, and not the cause. Therefore, these associated problems should be thoroughly analyzed and treated.
Ethical approval
Written approval and consent to participate was obtained from all study participants. If the participant was illiterate, an informed consent was obtained from a legal representative. The study protocol adhered to the tenets of the declaration of Helsinki, and was approved by the Research Ethics Committee of the Federal University of Technology of Paraná (UTFPR), CAAE 13698218.8.0000.5547.