Introduction
The issue of high-risk pregnancies is gaining importance in high-income, developed countries. This is due to several factors, such as advanced maternal age, the greater spread of assisted reproductive technologies, and an increase in comorbidities like hypertension, diabetes, or autoimmune diseases. It is estimated that about 12% of pregnancies are higher-risk [1,2]. A high-risk pregnancy implies a significantly elevated danger to maternal and fetal health, often requiring more frequent hospitalizations or outpatient visits [2,3]. These circumstances can lead to emotional distress, fear for the health of the mother and fetus, and a perceived loss of intimacy [4,5]. Consequently, pregnant women with high-risk conditions may feel more vulnerable and experience elevated stress [6,7]. Several studies have reported that depressive disorders can reach a prevalence of up to 44.2% among high-risk pregnancies, thus contributing to adverse maternal-fetal outcomes [8].
Despite this evidence, the psychological impact of long-term hospitalization or intensive obstetric surveillance has not been thoroughly investigated. Previous literature on high-risk pregnancies has explored social and psychological aspects, including women’s concerns, stressors, and support needs [9]. To expand upon these findings, we administered the Cognitive Behavioral Assessment Hospital Form (CBA-H) [10] psychological test to a cohort of hospitalized women.
We aimed to analyze the correlation between psychological factors (i.e. anxiety, depression, perceived stress) and environmental/clinical parameters (length of hospital stay, obstetric outcomes) in high-risk pregnancies.
Methods
Study design and setting
We conducted a cross-sectional study to evaluate the psychological implications of hospital care in women with high-risk pregnancies. The study was conducted at the Division of Gynecology and Obstetrics of the Department of Surgical Sciences, University of Cagliari (Cagliari, Italy), over 1 year (December 2016–October 2017).
Eligibility Criteria
The inclusion criteria were:
- Pregnant women with a confirmed high-risk condition (i.e. threatened preterm delivery, preeclampsia, placenta previa, or other significant complications).
- Required hospitalization for ≥ 7 days.
- Fluent in Italian and able to complete the questionnaire.
The exclusion criteria were:
- Hospital stay <7 days.
- Known psychiatric disorders or use of psychotropic drugs.
- Language barriers preventing reliable questionnaire completion.
Data collection
We collected maternal characteristics using a detailed anamnestic form following signed informed consent. The form covered:
- Sociodemographic data: age, ethnicity, marital status, education level, occupation, place of residence, and family/partner characteristics.
- Obstetric data: current pregnancy details, previous pregnancies, abortions, previous obstetric complications, and/or use of assisted reproductive technology (ART).
- Clinical data: personal and family history of chronic or psychological illnesses.
- Emotional/social data: presence or absence of emotional support during pregnancy, partner/family involvement, and time spent trying to conceive.
Psychological assessment (CBA-H)
The standardized CBA-H was administered to assess emotional and behavioral problems related to the clinical conditions. This questionnaire adapts the widely-used CBA-2.0 in health psychology, rehabilitation medicine, oncology, and pain therapy. The CBA-H enables healthcare professionals to identify emotional states and behavioral changes resulting from hospitalization and to establish connections with the patients' pre-existing characteristics, expressive modalities, and lifestyles.
It consists of 152 short and easy-to-read items with a dichotomous response format ("True" / "False"). The questions are divided into four forms, each examining different contexts.
Form "A" includes 21 items that explore the patient's emotional state at the time of filling out the test, including anxiety, depression, fears related to their health, and concerns related to hospitalization. The "A" sheet is divided into three scales (A1, A2, and A3). It provides three scores that quantify the state of anxiety, fears related to the patient's health conditions at the time of the test, and the possible presence of depressive reactions.
Form "B" includes 23 items that examines the emotional state, psychophysiological disorders, and manifestations of stress in the three months before hospitalization. It is divided into three scales (B1, B2, and B3) and investigates emotional and psychological aspects perceived over the last three months.
Form "C" includes 61 items that analyzes behavioral characteristics such as introversion and extroversion, emotional stability and instability, anxiety, irritability and impatience, hostility and social rigidity, and workplace involvement. It was designed to explore various personality traits and dimensions and the characteristics that reflect more stable and permanent emotional and behavioral attitudes. Sheet "C" has two scales for measuring personality and eight for identifying the psychological trait variables.
Form "D" includes 47 items that collects biographical information, emotional and sexual relationships, eating habits, sleep, physical activity, smoking or alcohol, satisfaction, and type of work. It is responsible for qualitatively analyzing habits and behaviors considered at health risk and investigating the quality of the individual's emotional, sexual, occupational, and social life.
Study registration, ethical and methodological standards
The study conformed to the methodological standards in the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement, available through the Enhancing the Quality and Transparency of Health Research (EQUATOR) Network [11]. In addition, the study design followed the Helsinki Declaration, conformed to the Committee on Publication Ethics (COPE) guidelines, and was approved by the university hospital’s Institutional Review Board (IRB), where it was performed.
Each participant was well informed about the procedures she had to undergo and signed an informed consent form for data collection for research purposes. Appropriate counselling was offered about the purpose of the study and the law’s guarantee of anonymous treatment of personal data, which guarantees privacy. Women were also informed about the opportunity to leave the observation freely whenever they considered it appropriate. Participation in the study protocol was strictly voluntary; no remuneration was offered for inclusion.
Statistical analysis
Patients’ characteristics are presented as mean ± standard deviation (SD) for continuous variables and frequencies (percentages) for categorical variables. Statistical analysis was performed using SPSS 20 (Chicago, IL, USA). Pearson’s correlation coefficient “r” calculation and the Student’s T test were used to evaluate associations and compare means. A p value <0.05 was considered as statistically significant.
Results
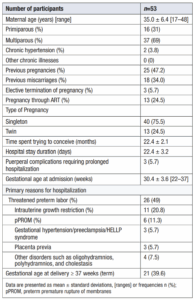
A total of 53 pregnant women met the inclusion criteria. The mean maternal age was 35.0 ± 6.4 years (range 17–48 years). Overall, 31% were primiparous, and 69% were multiparous. Two patients (3.8%) had chronic hypertension, but no other significant chronic illnesses were found.
The mean duration of hospital stay was 22.4 ± 3.2 days. Three cases of complications in the puerperium required prolonged hospitalization. The mean gestational age at admission was 30.4 ± 3.6 weeks (range 22–37 weeks). The leading causes of hospitalization included threatened preterm labor (n=26), intrauterine growth restriction (n=11), gestational hypertension/preeclampsia/HELLP syndrome (n=3), preterm premature rupture of membranes (pPROM, n=6), placenta previa (n=3), and other disorders (n=4) such as oligohydramnios, polyhydramnios, and cholestasis of pregnancy (Table 1).
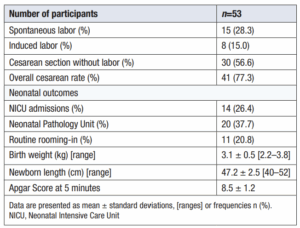
Table 2 shows neonatal outcomes, mode of delivery, and newborn characteristics in the study population.
The length of hospitalization negatively correlated with psychophysical well-being (B2) (Pearson’s r = –0.333).
The Apgar Score at 5 minutes was lower in babies whose mothers were admitted earlier in gestation (Pearson’s r = 0.567, p<0.001). In addition, as interpersonal difficulties (C8) increased, the Apgar score decreased (r = – 0.313, p=0.041). Gestational age at Admission was inversely related to birth weight and newborn length; earlier admissions tended to yield lower newborn weight and length (Table 2).
CBA-H Questionnaire results
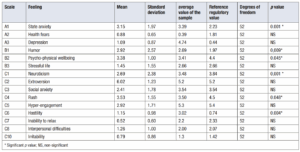
The CBA-H analysis revealed significant differences between the study sample and the normative population across multiple scales, highlighting the emotional and personality-related impact of hospitalization on high-risk pregnant women. Situational anxiety (A1) was significantly higher in the sample, with a mean score of 3.40 compared to 2.23 in the normative population, reflecting heightened emotional responses to the hospital environment. Depressive symptoms (A3) were also markedly elevated, with a mean score of 4.74 versus 0.44, suggesting that prolonged hospitalization exacerbated mood disturbances. Conversely, health-related fears (A2) were notably lower in the sample, with a mean score of 0.39 compared to the normative value of 1.81. This unexpected finding may indicate improved communication and trust in healthcare providers during extended stays, thus mitigating health-related anxieties.
The analysis also showed significantly higher scores for reduced mood (B1), with a sample mean of 2.69 compared to 1.97 in the normative group, pointing to persistent emotional distress. However, psychophysical well-being (B2) showed a slight improvement, possibly reflecting some adaptation to the hospital environment. While elevated, stressful life events (B3) did not reach statistical significance. Neuroticism (C1) was significantly elevated among personality-related traits, indicating increased emotional instability. Impulsivity or urgency, as measured by the “Rush” scale (C4), was considerably lower in the sample compared to the normative population (3.50 vs. 4.50), suggesting that the structured hospital environment reduces the need for rapid decision-making or urgent responses. Social anxiety (C3) and hostility (C6) were also significantly higher in the sample, indicating interpersonal and emotional challenges faced by the participants. However, interpersonal difficulties (C8) and irritability (C10) did not differ statistically. Table 3 shows mean scores across the CBA-H scales.
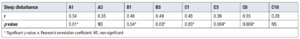
Sleep disturbances also emerged as a critical factor influencing psychological well-being, as summarized in Table 4. Significant correlations were observed between sleep disturbances and several CBA-H scales. Situational anxiety (A1) exhibited a moderate positive correlation with sleep disturbances (r = 0.343, p = 0.012), while depressive symptoms (A3) showed a similar association (r = 0.35, p = 0.015). Reduced mood (B1) and social anxiety (C3) were also significantly correlated with sleep disturbances (r = 0.469, p = 0.045; r = 0.39, p = 0.004, respectively). These findings underscore sleep's critical role in modulating emotional and interpersonal functioning during hospitalization.
Discussion
The findings of this study highlight the profound psychological impact of hospitalization on high-risk pregnant women, underscoring the need for comprehensive care that addresses both medical and emotional well-being. Elevated levels of situational anxiety (A1) and depressive symptoms (A3) align with previous research on the emotional toll of high-risk pregnancies and prolonged hospitalization. These psychological stressors not only affect maternal mental health but are also associated with poorer perinatal outcomes, emphasizing the importance of early psychological interventions.
Interestingly, the significantly lower scores for health-related fears (A2) in this population suggest that prolonged contact with healthcare providers may foster trust and alleviate anxieties about maternal and fetal health. This finding highlights the potential for effective communication and supportive patient-provider relationships to mitigate specific psychological stressors. Future interventions could strengthen these relationships through transparent and empathetic communication strategies.
The results revealed a significant reduction in the “Rush” scale (C4), indicating that the structured hospital environment likely reduces the urgency and impulsivity typically driven by external stressors. While this finding underscores the calming effect of a controlled medical setting, it also raises questions about the potential for patients to feel a loss of autonomy. Balancing the benefits of structured care with the need to preserve patients’ sense of control is critical for minimizing emotional distress and fostering resilience during hospitalization. Future research should explore strategies to enhance patient autonomy, such as shared decision-making models and personalized care plans.
Another notable finding was the significant correlation between poor sleep quality and emotional states, including situational anxiety, depressive symptoms, and reduced mood (B1). This highlights the critical role of sleep in emotional regulation and psychological well-being. Given the impact of poor sleep on emotional and interpersonal functioning, interventions targeting sleep disturbances—such as relaxation techniques, sleep hygiene education, or cognitive-behavioral therapy for insomnia—could be particularly beneficial for hospitalized high-risk pregnant women.
Although interpersonal difficulties (C8) and irritability (C10) did not show statistically significant differences, their slight elevation in the sample warrants attention. While not prominent, these traits could still influence hospital experience and interactions with healthcare providers. Tailored interventions addressing interpersonal and emotional challenges, such as group therapy or mindfulness-based programs, could help mitigate these issues and enhance patient-provider communication.
The study also emphasizes the importance of addressing psychological traits like neuroticism (C1) and hostility (C6), which were significantly elevated in the sample. These findings suggest that high-risk pregnancies may exacerbate emotional instability and vulnerability to interpersonal conflict. Psychological support tailored to these traits, such as individual counseling or stress management programs, could help patients develop healthier coping mechanisms and improve their hospital experience.
Finally, the correlation between early hospitalization and poorer neonatal outcomes, including lower Apgar scores and reduced birth weight and length, underscores the interplay between maternal psychological well-being and perinatal health. These findings further support the need for integrated care models that address simultaneously the psychological and medical needs of high-risk pregnancies.
The results of this study highlight the need for standardized psychological screening and support protocols in high-risk obstetric settings. Implementing routine assessments with validated tools like the CBA-H could help identify vulnerable patients early and guide targeted interventions. Programs addressing sleep disturbances and fostering patient autonomy could enhance emotional resilience and improve maternal and neonatal outcomes. Future research should explore the long-term psychological impact of high-risk pregnancies and assess the efficacy of integrated care models that include psychological, medical, and social support components. Additionally, postpartum follow-up should evaluate the persistence of psychological effects, particularly the risk of postpartum depression, in this vulnerable population.
Strengths and limitations
A strength of this pilot study is its detailed exploration of emotional/behavioral dimensions using a standardized tool (CBA-H). However, the sample size (n=53) is relatively small, limiting the generalizability of the results. We also did not assess postpartum mood disorders (i.e. postpartum depression) or follow participants beyond the immediate puerperium. Another limitation of this study is the lack of a comparison group of pregnant women with complications but without hospitalization. We acknowledge that pregnancy complications themselves may have an impact on the psycho-emotional state, making it difficult to attribute the observed effects solely to hospitalization. Future studies should consider including a control group of pregnant women with complications who were not hospitalized, or those hospitalized for preventive purposes or routine examinations, to further clarify this aspect. In addition, future studies should include larger cohorts, longitudinal designs, and postpartum follow-up.
Clinical implications and future directions
Our findings emphasize that long-term hospitalized high-risk pregnant women require comprehensive care addressing both physical and psychological well-being. Midwives play a pivotal role in establishing a trusting therapeutic relationship, recognizing signs of psychological distress, and facilitating referrals to mental health services [12]. Postpartum follow-up should also evaluate the potential onset of postpartum depression, especially in those who exhibit heightened anxiety or depressed mood during pregnancy [13].
Conclusions
High-risk pregnancies inherently heighten vulnerability to psychological stressors such as anxiety, depression, and hostility, which can significantly impact both maternal and neonatal outcomes. Prolonged hospitalization, while medically necessary, may exacerbate these emotional challenges, underscoring the need for a holistic care approach. This study highlights the importance of integrating routine psychological screening and tailored support interventions into the care of hospitalized pregnant women.
A multidisciplinary approach involving obstetricians, midwives, psychologists, and social workers is essential to comprehensively address this vulnerable population's complex emotional, social, and physical needs. Such integrated care not only promotes maternal mental health but also contributes to improved perinatal outcomes. Future research should focus on developing and implementing standardized psychological support protocols and evaluating the long-term benefits of these interventions for both mothers and their newborns.
Authors Contribution
S.D.M. drafted the work and made substantial contributions to the conception, design, analysis, and interpretation of data, revising it critically for important intellectual content and final approval of the version to be published.
C.O. contributed to the acquisition and interpretation of data, ensuring that questions related to the accuracy or integrity of any part of the work were appropriately investigated and resolved and finally approved the manuscript version to be published.
A.C. critically revised the work for important intellectual content and gave approval for the publishing of the final version.
A.V. critically revised the work for important intellectual content and gave approval for the publishing of the final version.
A.R. critically revised the work for important intellectual content and gave approval for the publishing of the final version.
S.A. contributed substantially to the conception and design of the work supervision and approved the final version of the manuscript for publication.