Introduction
During reproductive life vaginal discomfort (VD) is frequently claimed by women as a factor worsening their quality of life. VD is mainly induced by vaginal discharges, burning and itching of genitalia, and it represents the primary reason for gynecological consultation, in different medical settings [1]. Causes of VD are recognized under the umbrella diagnosis of vaginal infections which could be sustained by bacteria, fungi and protozoa local infection. Bacterial vaginosis (BV) is the most prevalent while either vulvovaginal candidiasis (VVC) and Trichomonas infections account for the vast majority of the remnant cases [2].
Although BV can be efficaciously treated with proper antimicrobial agents, metronidazole representing the gold standard [3], this condition is characterized by frequent relapses and the recurrence of VD requires different approaches. Among them, pH changes and biofilm disruption have provided moderate quality of evidence in terms of benefit, in addition to either barrier or hormone contraception [4].
On the other hand, few attention has been focused on the fact that most of the bacterial species sustaining BV (Gardnerella vaginalis, Atopobium vaginae, Megasphera, Prevotella and Sneathia) are classified as anaerobia bacteria since their proliferation could take place only in the absence of oxygen. Indeed, the presence of oxygen in the environment induced a block of bacterial growth [5]. Although Lactobacillus spp are included among anaerobia, they are still aero-tolerant and insensitive to oxygen exposure [6].
Vaginal oxygen supplementation has recently been proposed as a treatment for some gynecological disorders. Once coupled with hyaluronic acid, cycles of vaginal oxygenation gave definite therapeutic benefits in a cohort of patients with relapsing episodes of VVC [7]. Similarly, the same combo improved vaginal atrophy in postmenopausal women [8] as well as sexuality and urinary symptoms in breast cancer survivors, both in fertile or postmenopausal age [9].
On these grounds, we performed a pilot, randomized, controlled trial aiming to verify the effects of vaginal oxygen supplementation in a group of women affected by VD due to vaginal infections.
Methods
This was a pilot, randomized, controlled, open label, monocentric trial in which women of fertile age presenting for VD were screened and those reaching a diagnosis of vaginal infections were enrolled, after informed consent was obtained.
Inclusion criteria were: age 18-45 years, diagnosis of vaginal infections of different etiology, ability to fill-in the symptom’s sheet and the comprehension of the informed consent sheet. Exclusion criteria were: vulvo-vaginal atrophy, amenorrhea since at least 3 months and exposure to antibiotics in the previous 30 days.
Each woman received a general physical and gynecological examination at entry to the study, together with a vaginal swab. Moreover, the subjects rated their VD on a Likert scale evaluating vaginal discharges, vulvovaginal itching/burning and dyspareunia. Once inclusion and exclusion criteria were met, subjects underwent a randomization (1:1:1) in three different groups of intervention. Randomization was managed by a midwife who used sealed envelopes containing treatment allocation that was performed through a random series of numbers. Treatment was disclosed after the patient’s consent was signed.
Group A received vaginal high concentration oxygen supply (O2 concentration >95%, 3 lt/min for 20 minutes), twice/week for 2 weeks; group B received vaginal oxygen as Group A added to a targeted antibiotic or antimycotic treatment for 5-7 days; and Group C (control group) receive the targeted antibiotic or antimycotic treatment for 5-7 days.
The oxygen treatment was carried out using the Caress Flow system (Caress Flow - Bologna, Italy), an oxygen therapy device for gynecological use that allows the topical administration of oxygen through a vaginal cannula with a high degree of purity and a flow rate of 3 lt/min.
Both vaginal swab and symptoms ratings were performed 10-14 days after the end of treatment. Women self-rated vaginal itching/burning, vaginal discharges and dyspareunia on a Likert scale from 0 (absent) to 10 (maximal discomfort), as performed at entry in the study.
The primary outcome was a composite VD score obtained from the sum of vaginal discharge, vaginal itching/burning and dyspareunia. Secondary outcomes were the individual components of the VD score.
Due to the explorative nature of the study, the sample size was determined a priori as being composed by 36 women, 12 each group.
Statistical analysis was performed by comparing Groups through parametric and non-parametric tests when appropriate, according to the distribution of data. Percent variations were also calculated and compared through ANOVA. A p value of < 0.05 was considered statistically significant.
Results
Out of 36 randomized women 32 were analyzed. Two women immediately retired consent and further two were lost after first contact not presenting to follow-up.
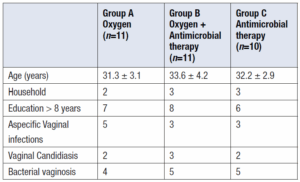
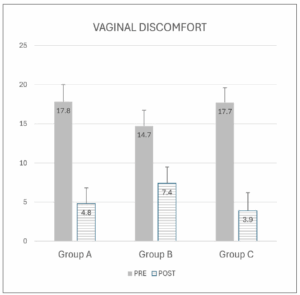
The clinical features were not different among the randomized women (Table 1). At baseline, the total VD score was similar among the 3 groups (Figure 1). Similarly, there were no differences in the rating of baseline symptoms such as vaginal itching/burning (Kruskall-Wallis [KW] =1.696, d.f. 2.32; p=0.428), vaginal discharge (KW = 1.266, df. 2.32; p=0.531 and dyspareunia (KW=0.500, d.f. 2.32; p=0.779) among the 3 groups.
VD was significantly reduced by treatment in all the 3 groups (Figure 1). Indeed, VD score was significantly reduced by 89.2 ± 7.1% in Group A, by 85.1 ± 10.1% in group C and to a lesser extent by 52.8 ± 9.2% in group B.
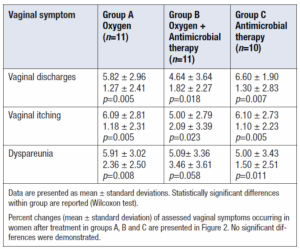
Vaginal symptom scores before and after treatment are presented in Table 2. Vaginal discharge and itching/burning score were significantly reduced in every group after treatment. Dyspareunia was not significantly reduced in women receiving both oxygen and antimicrobial therapy (Table 2).
Data are presented as mean ± standard deviations. Statistically significant differences within group are reported (Wilcoxon test).
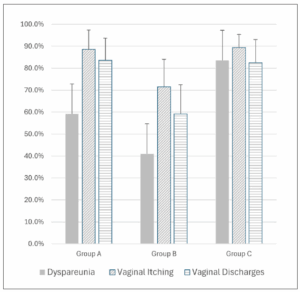
Percent changes (mean ± standard deviation) of assessed vaginal symptoms occurring in women after treatment in groups A, B and C are presented in Figure 2. No significant differences were demonstrated.
Discussion
This pilot, controlled trial demonstrated that vaginal oxygen delivery is associated with a reduction of the main vaginal discomfort symptoms, i.e. discharges, itching as well as dyspareunia, in women affected by vaginal infections of diverse etiologies. The efficacy extent of vaginal oxygen was not different respect to the standard antimicrobial approach alone or in combination with oxygen.
In the present series the most part of the patients either presented with BV or with candidiasis. Our data confirmed that targeted treatment (antibiotics or antimycotics) is able to reduce symptoms and restore vaginal health [10]. However, literature has reported that there are several limitations in the use of antimicrobial agents. Firstly, vaginal infections frequently relapse, hence requiring recurrent treatments, with over exposure to the drugs [11]. Secondly, the use (and abuse) of these agents is associated with the development of microbial resistances that now become a public health issue on a global scale [12].
For the above reasons it is of paramount importance to look for alternative treatments. Among tested interventions, there are pH modulators such as lactic acid <{13], with few, if any effects, antiseptics like boric acid [14], also with few, if any effects), changing diet [15],, with few benefits, and probiotics. These last products have gained attention in the last years when added after the antimicrobial agent [16], or alone {17,18]. Unfortunately, results are still heterogeneous to guide an evidence-based approach being closely depending on the quality and quantity of bacterial strains of each product.
Anaerobic bacteria, namely those sustaining BV, are naturally vulnerable to oxygen. Indeed, aerobiosis stimulates the formation of reactive oxygen species, interferes with the redox processes necessary for their physiology and ultimately arrest their proliferation [19]. For those reasons, hyperbaric oxygen was established as a treatment in cases of clostridial myonecrosis, necrotizing soft-tissue infections, myocarditis and so on [20]. Moreover, oxygen promotes tissue repair, thus stimulating angiogenesis through vascular endothelial growth factor [21].
Just recently the interest towards a local oxygen treatment has arisen. In vitro, antimicrobial oxygen activity on P. gingivalis has been reported in patients affected by periodontitis where the treatment could foster eubiosis [22]. On the other hand, the application of local normobaric high concentration oxygen through vaginal insufflation was previously reported useful for relieving the urogenital syndrome once associated with hyaluronic acid, in postmenopausal breast cancer survivors [9].
In view of previous clinical experiences and experimental observations we could hypothesize that oxygen action is exerted at different levels, i.e. inhibition of microbial growth, removal of biofilms and promotion of reparative processes.
This study has some limitations inherent to the small sample and to the fact the sample size was not calculated due to the pilot nature of the investigation. Moreover, different types of vaginal infections were included not allowing to draw conclusion inherent to each one of them. However, we could foresee that oxygen effect would be better exploited in cases of BV to avoid relapses.
In conclusion, the efficacy and tolerability of vaginal oxygen insufflation in the treatment of vaginal infections is here reported for the first time. The clinical short-term effect is not different to the conventional antimicrobial approach. Larger studies with longer follow-up are required to confirm these first pilot observations.