Introduction
Urinary incontinence is a common and distressing condition affecting a significant proportion of women worldwide [1,2]. Stress urinary incontinence (SUI) involves involuntary urine loss during physical activity or conditions that increase intra-abdominal pressure such as coughing or sneezing. Urge urinary incontinence (UUI) is the inability to hold urine when the urge strikes, while mixed urinary incontinence (MUI) combines both types [1,2]. Epidemiological studies estimate the prevalence of urinary incontinence at 25% in young adults and 45% in older women [3].
The etiology of SUI is multifactorial, involving weakened pelvic floor muscles and/or connective tissue, or deficient urethral sphincter [1,2]. UUI is associated with overactive bladder syndrome and involuntary detrusor muscle contraction [1,2]. Pelvic floor muscle training (PFMT) is the recommended first-line therapy for SUI, and, when combined with bladder training or antimuscarinics, also for UUI [3,4]. While PFMT achieves a subjective cure in ~50% of cases, it often fails due to inadequate guidance and compliance [5]. Secondary conservative options include electrical stimulation, vaginal devices, and urethral inserts. Women with severe symptoms often choose surgery, while those with milder symptoms prefer non-surgical treatments that prioritize safety and recovery [6].
Recent therapeutic advancements offer improved efficacy and minimal invasiveness for SUI treatment. Non-ablative Erbium:Yttrium-Aluminum-Garnet (Er:YAG) laser therapy strengthens pelvic floor connective tissue [7] by delivering thermal energy to the vaginal mucosa, enhancing collagen structure and stimulating new collagen production [8,9]. Clinical studies report healing/improvement rates of 38-78% at 6-month follow-ups [10–13]. A randomized, sham-controlled study demonstrated significantly (p<0.001) greater reductions in International Consultation on Incontinence Questionnaire-Urinary Incontinence Short Form (ICIQ-UI SF) scores in the laser group versus sham [14]. A multi-center randomized trial further confirmed the efficacy and safety of Er:YAG laser treatment for SUI [12].
Functional magnetic stimulation or High Intensity Tesla magnetic Stimulation (HITS), is a non-invasive treatment for SUI that improves muscle function without obvious side effects [15–19]. It uses passive magnetic waves to stimulate sacral roots or pelvic floor muscles, inducing contraction—ideal for patients unmotivated to do regular PFMT [16,19]. A meta-analysis reported better objective and subjective cure rates and improved micturition in patients receiving active stimulation [16].
While both non-ablative Er:YAG laser and functional magnetic stimulation/ HITS therapy show promise for SUI treatment, to our knowledge, no studies have explored their combined effects. Given their distinct tissue targets—laser for connective tissue and HITS for pelvic floor muscles—this study investigated the potentially complementary effect of combining these therapies for women with SUI. Given the overlapping symptoms of stress and urgency incontinence in women with MUI, and the emerging efficacy of magnetic stimulation in treating urge symptoms [18,20], we included women with MUI when SUI symptoms were prevalent.
Methods
This investigator-initiated, single-arm pilot study was conducted at Zdravstveni Zavod Štrumbelj (Ljubljana, Slovenia), approved by the Slovenian Ethics Committee (No. 0120-44/2021-3), and registered at ClinicalTrials.org (NCT06559423). Participants (24 women, aged ≥18 years) with clinically diagnosed SUI or MUI (SUI predominant), were recruited from April to August 2021 in a urogynecological practice (see Supplementary material for exclusion criteria). The sample size was determined based on established recommendations for pilot studies [21]. All participants were informed of the study and gave written informed consent to participate.
Combined laser and HITS treatment
Three monthly Er:YAG laser sessions (TimeWalker® IntimaLaser™, Fotona, Slovenia) followed the IncontiLase® protocol—treating the anterior vaginal wall, the entire vaginal canal and the vestibule and introitus. Six weeks after the final laser session, six HITS treatments (StarFormer®IntimaWave®, Fotona, Slovenia) were delivered twice weekly with intensity tailored to patient tolerance (See Supplementary material for details).
Evaluation of symptom improvement
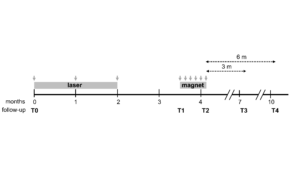
Symptom severity was assessed at baseline (T0), week 14 (T1), week 16 (T2), and at 3 (T3) and 6 months (T4) after the treatment (Figure 1) using three questionnaires: the ICIQ-UI SF, the Questionnaire for Urinary Incontinence Diagnosis (QUID), and the Female Sexual Function Index (FSFI). ICIQ-UI SF measures SUI severity (frequency and amount of urine loss) [22] with higher scores indicating more severe SUI. A minimum important difference (MID) of -2.52 represents clinical relevance [22,23].
The QUID diagnoses incontinence type, with cutoff scores of ≥4 for SUI and ≥6 for UUI and values above both cutoff scores indicating MUI [24]. The FSFI assesses six domains of sexual function, with scores ˂26.55 indicating female sexual dysfunction (FSD) [25]. See Supplementary material for more details. Pelvic floor muscle strength was assessed by palpation and the modified Oxford scale. Treatment-related pain and safety outcomes were evaluated at each visit using a 10-point visual analog scale (VAS) pain score and safety assessments. The Patient Global Impression of Improvement (PGI-I) questionnaire assessed perceived improvement using a Likert scale.
Statistical analysis
The data were analyzed using IBM SPSS Statistics (version 29.0), following the intention-to-treat principle. Data are presented as frequencies n (%), mean ± standard deviation (SD) or median [minimum, maximum values]. Normality of data distribution was assessed using the Shapiro-Wilk test. Normally and non-normally distributed variables were respectively analyzed using ANOVA and the Friedman repeated measure tests (both with Bonferroni correction). Categorical variables were analyzed using the Fisher exact test in GraphPad Prism 9. A significance level of p<0.05 was applied.
Results
Twenty-four women (average age 42.7 years; Table S1) with moderate to severe SUI or MUI (SUI predominant) underwent the laser and HITS treatment regimen as shown in Figure 1.
Primary outcomes
The study’s primary outcomes were the efficacy and safety of the combined treatment. Efficacy was assessed using two self-assessment questionnaires, the ICIQ-UI SF and the QUID. While both questionnaires measure symptom severity, the ICIQ-UI SF assesses the impact of incontinence on quality of life [22] and the QUID diagnoses incontinence type [24].
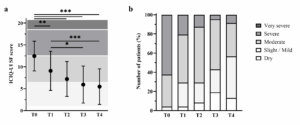
At baseline (T0; n=24), ICIQ-UI scores indicated the one patient had mild SUI (4.2%), 8 (33.3%) moderate, and 15 (62.5%) severe, with an average score of 12.46 ± 3.40 (Tables S1 and S2, Figure 2). Symptoms improved significantly after combined therapy (p<0.001) and persisted for 6 months (p<0.001), with a mean score of 5.48 ± 4.06 (Figure 2a, Table S2). At 6 months, 3 patients out of 23 who filled out the questionnaire (13.0%) were dry, 10 (43.5%) had mild, 8 (34.8%) moderate, and 2 (8.7%) severe symptoms (Figure 2b). Severe SUI symptoms decreased after laser therapy (T1), shifting towards mild and moderate symptoms (Figure 2b). While no significant improvement occurred at the final HITS therapy session (T2) compared to T1, symptoms improved significantly at the 3- and 6-month follow-ups (Figure 2a, Table S2). The reduction in ICIQ-UI scores exceeded the -2.52 MID threshold at all time points (Table S3).
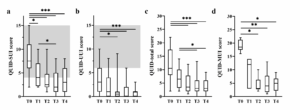
At baseline, QUID showed that 22/24 patients had SUI, 7 had UUI, and 6 had both (Table S4). Median QUID-SUI and QUID-UUI scores were 7.5 (min 2, max 15) and 3 (min 0, max 9), respectively (Tables S1 and S2). After laser treatment (T1), SUI scores improved significantly (p<0.05) (Figure 3a), but not UUI, total QUID, or MUI scores (Figure 3 b, c and -d, Table S2). After HITS treatment (T2), all QUID domains improved significantly (p<0.05), with effects persisting up to 6 months (SUI: 3 [min 0, max 8] and UUI at 1 [min 0, max 3]).
On the 10-point VAS assessing pain, patients reported moderate initial pain during laser therapy, which decreased over subsequent sessions. Median pain scores for laser treatment were 7 (min 2, max 9), 4 (min 0, max 8) and 2.5 (min 0, max 8) for the first, second and third sessions, respectively. Local anesthetic was used in only 5 of 72 sessions and post-treatment hyaluronic acid was rarely applied. HITS treatments were pain-free (VAS = 0). Minimal vaginal discharge (2 patients post-laser, 1 post-HITS) and vaginitis (1 post-laser, 2 post-HITS) were the only reported adverse effects.
The median pre-treatment FSFI score (Table S1) assessing overall sexual function was below the FSD threshold (grey area, Figure S1). Scores improved significantly (p<0.01) at 6 months, surpassing the FSD level, with all FSFI domains showing improvement (Table S5).
Pelvic floor muscle strength was assessed throughout treatment. At baseline (T0), 77% of women had weak, flickering, or absent contraction (Table 1). After laser treatment (T1), 21% improved, but 71% remained weak or worse. Post-HITS (T2), 83% showed significant improvement (p=0.002; Tables 1 and S6). At the 3- and 6-month follow-ups, >70% had moderate, good, or strong contractions (Table 1), significantly higher than the baseline 23% (p<0.05, Table S6).
According to the PGI-I scale, the percentage of participants reporting that they were “very much better” increased steadily from 29% after laser treatment (T1) to 61% at the 6-month follow-up (T4) (Table 2). The overall percentage of patients reporting any degree of improvement (“a little better” to “very much better”) also remained consistently above 90% at all time points, with 96% of women reporting sustained improvement at 6 months (Table 2).
Discussion
Female urinary incontinence significantly impairs quality of life and requires tailored interventions for SUI and UUI [1,2,4]. PFMT often fails due to non-compliance, while emerging treatments like non-ablative Er:YAG laser therapy and functional magnetic stimulation offer promising minimally invasive alternatives [12,14,26,27]. This pilot study investigated the efficacy and safety of three laser sessions combined with six HITS sessions in 24 women with SUI or MUI (SUI predominant). ICIQ-UI SF and QUID scores showed significant improvement, in line with clinically relevant symptom alleviation lasting up to 6 months (Figures 2 and 3, Table S3). Symptoms improved in ~50% of patients after laser treatment, 71% after HITS treatment and >90% 6 months post-treatment. Overall, >90% of participants reported reduced SUI symptoms at 6 months (Table 2). While laser improved SUI, HITS further improved UUI and MUI (Figure 3). The dual nature of MUI requires treating both SUI and UUI, which can be challenging [4]. The observed improvement in UUI after HITS therapy is consistent with previous studies showing that magnetic stimulation can reduce detrusor overactivity and urgency symptoms in women with UUI or MUI [18,20]. Improvements in female sexual function (Figure S1 and Table S5) underscore the multiple benefits of combined therapy.
Previous studies comparing laser treatment with sham or PFMT showed inconclusive results on muscle contraction strength [14,28], and a study without a control group found no effect on pelvic muscles [29]. In our study, most women initially had weak or absent pelvic floor strength, which improved significantly after the treatment (Tables 2 and S6). The non-ablative Er:YAG laser stimulates collagen remodeling and neocollagenesis, which can persist for several months post-treatment [7,8], thus, promoting tissue tightening. However, the relatively low penetration depth of the laser-induced heat (a few hundred micrometers) [30], limits its impact on muscle contraction. In contrast, HITS therapy enhances cellular repair and muscle function, as shown by perineometry and electromyography data [17,19,26,27]. The present study suggests that even severe SUI cases may benefit from combined therapy (Figure 2b), with encouraging symptom improvements as observed in a pilot setting [10]. However, as this treatment may not cure incontinence but rather alleviate its symptoms, it is important that patients—especially those with severe symptoms—be appropriately counselled as part of the shared decision-making process. Clear communication about treatment will help patients make an informed choice between non-invasive symptomatic options and definitive surgical treatments.
Safety evaluation showed that both laser and HITS treatments were well tolerated, with no unexpected adverse effects and generally low pain scores, consistent with previous findings [19,31]. This suggests that the combined therapy is safe and tolerable for SUI or MUI patients. A reduction in urinary incontinence episodes and improved quality of life highlight the potential synergistic effects of a combined therapy. Recent research has also shown that combining intravaginal and intraurethral Er:YAG laser therapies is particularly effective, especially in postmenopausal women, providing better SUI relief than intravaginal laser alone [32,33]. Combining different procedures—such as intravaginal and intraurethral laser therapies, or intravaginal laser with HITS—may offer a more comprehensive approach to SUI management, but more studies are needed to validate these strategies. The sequential administration of Er:YAG laser and HITS allowed us to observe the distinct benefits of the two therapies. Er:YAG laser treatment is minimally invasive, offering moderate symptom relief through tissue remodeling, but has limited effect on the deeper muscle structures. HITS, in contrast, actively strengthens the pelvic floor muscles and showed greater improvements in continence, although it requires more time and patient engagement. Future studies should investigate the potential benefits of simultaneous therapy, as compared to the sequential approach. While the combination of Er:YAG laser and HITS shows promise with sustained efficacy, safety, and improved sexual function, the study's limitations—including a small sample size, lack of a control group, risk of bias, and relatively young participants—highlight its preliminary nature.
Further randomized controlled studies with larger cohorts and longer follow-up periods are warranted to demonstrate the potential synergies between these innovative, non-invasive treatments.
Author’s contribution
Tadeja Štrumbelj and Tina Logar1 designed the study, collected the data, analyzed the data and drafted, revised and approved the final manuscript.
Data availability statement
The data that support the findings of this study can be made available from Tina Logar upon reasonable request.
Supplementary material
A PDF file of supplementary material for this paper is available (Strumbelj_Supplementary Material).