Introduction
Breast adenomyoepithelioma (AMEB) is an infrequent breast tumor characterized by proliferation of both epithelial and myoepithelial cells, presenting a characteristic biphasic pattern. AMEs are classified as a subtype of epithelial-myoepithelial lesions [1]. The majority of AMEB are benign and have a good prognosis. However, malignant transformation has also been described and can be of one or both components (epithelial and or myoepithelial cells). Malignant AMEB (MAMEB) is an entity with potential for local recurrence and distant metastasis [1-5].
To date, less than 100 cases of MAMEB have been reported in the literature [3,4]. For this reason, MAMEB still remains poorly understood and there is not a standardized definition and therapeutic approach in international guidelines. Furthermore, predictive features of malignancy are still unknown [1,2,4,6].
According to the management performed in the scarce published cases, it is recommended to perform a complete excision of the lesion at early stage with clear margins. However, adjuvant treatment regimens have not been established, with no evidence available regarding the role of axillary lymph node dissection, chemotherapy nor radiation therapy [1,2,4].
We present a case of a MAMEB treated in our institution, and provide a brief review of its management due to its unusual presentation.
Case report
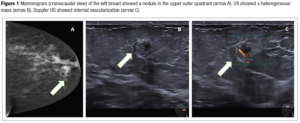
A 61-year-old woman was referred to our center after detecting a nodule in her left breast in a screening mammography (Figure 1, BIRADS 4). The patient was asymptomatic and had no relevant medical history. Regarding family background, her mother was diagnosed with colorectal cancer at 62 years of age and died 2 years later.
No breast nodules or any palpable axillary lymph nodes were reported at physical examination. Breast ultrasound (US) showed a subcutaneous 10-millimeter heterogeneous circumscribed round mass in the upper outer quadrant of the left breast. Power Doppler image showed internal vascularization of the lesion (BIRADS-4B). Breast magnetic resonance imaging (MRI) was conducted, revealing a 10 mm nodule in the upper external quadrant of the left breast, without diffusion restriction upon dynamic study (apparent diffusion coefficient 1.6; BIRADS-4B).
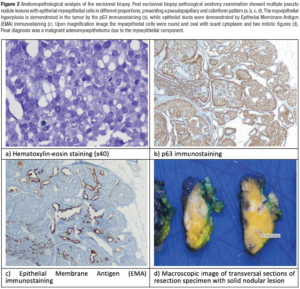
Axillary US showed no suspicious lymph nodes. An US-guided 14 G core needle biopsy was performed, obtaining a biphasic proliferation of epithelial and myoepithelial cells with cytological atypia and mitosis figures with a ki67 proliferation index of 30%, that suggested, as the first diagnostic option, a MAMEB due to the myoepithelial component. Extension study showed no signs of distant metastasis.
After multidisciplinary Tumor Board discussion wire-guided lumpectomy was performed and final pathological specimen analysis confirmed a MAMEB with a malignant myoepithelial component of 10 mm (Figure 2). Margins were assessed and considered negative (nearest margins were at 2 mm and 3 mm).
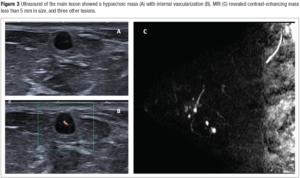
After surgery, a one-year follow-up mammogram was performed (Figure 3-A). A new 5-mm round nodule was identified in the upper outer quadrant of the left breast. On this occasion, the lesion was also subcutaneous, but hypoechoic on US, with internal vascularization (BIRADS-0, Figure 3-B). A thorough US examination of the outer quadrants showed three similar lesions smaller than 5 mm in size (BIRADS-4B). Core needle biopsy of the main lesion revealed myoepithelial proliferation without cytological atypia nor mitosis figures. MRI showed four contrast-enhanced masses (BIRADS-4, Figure 3-C).
Discussion and literature review
AMEB was first described in 1970 by Hamperl [7] as a rare neoplasm, which to date in the literature or international guidelines there is no clear description of its management [4,5]. According to the World Health Organization (WHO), breast AMEB can be classified into benign and malignant subtypes [4,8,9]. Most AMEB are benign and have a good prognosis. Malignant AMEB (MAMEB) incidence is low, with less than 100 cases described in the literature [3,4], and are characterized by a possible aggressive behavior [1,2,4,6,8].
Epidemiology and classification
A recent work by Rakha et al. [10] suggested the classification of AMEB as benign, atypical and malignant; moreover, MAMEB are subclassified based on histologic findings into in situ MAMEB (when it has a malignant epithelial component showing Ductal Carcinoma In Situ features), invasive MAMEB (when malignancy affects epithelial, myoepithelial or both components) and invasive MAMEB with carcinoma (when malignancy is due to epithelial features that are similar to conventional invasive breast cancer). This classification is based on their histopathological and clinical features but has not been validated so far [10]. Regarding its clinical presentation, MAMEB mostly occur in middle-aged women and are usually manifested as a palpable lump with a rapid growth pattern at presentation [5,6,8].
Considering its potential for local recurrence and distant metastasis, MAMEB can also present infiltration of peripheral tissues or metastasis in other organs such as lungs, thyroid gland, bones and brain [2-4,8].
Diagnosis
Diagnosis of MAMEB is challenging, not only due to its exceptionality, but also because morphological features of the tumor that could predict malignant transformation are not clearly described. Therefore, it seems that neoplasms diagnosed as benign AMEB may become malignant in time [1,2,4,8]. The diagnosis process of MAMEB combines imaging techniques, immunohistochemistry and histological features.
MAMEB can be observed in mammography and ultrasound examinations as a nodule or mass, although such findings tend to be unspecific and breast MRI may be performed to complete the study [5,8]. It has been reported that tumor size could be associated with malignancy, being recommended by some authors to treat all AMEBs larger than 2 cm as malignant [1,2].
Some histological characteristics have been associated to malignancy in MAMEB including: cellular and nuclear pleomorphism, high mitotic rate, hyperplasia of glandular epithelial or myoepithelial cells, abnormal nuclear division, high number of mitotic figures, cellular atypia, surrounding tissue invasion and necrosis. However, a clear reference to distinguish between benign and malignant AMEBThe case was discussed in the Tumor Board has not been established so far [1-5].
Immunohistochemistry provides valuable information for the diagnosis of MAMEB. Firstly, it helps to confirm the dual cell composition of the neoplasm. Myoepithelial cells are usually positive for high molecular weight cytokeratin, such as CK5/6 and CK14 p63, SMA (smooth muscle actin), CD10 and calponin. Epithelial cells tend to express low-molecular weight cytokeratin, such as CK7 and CAM 5.2, and EMA. Secondly, although the estrogen receptor (ER) and progesterone receptor (PR) immunostaining can be focally positive, around of 40% of AMEB are hormone receptor and HER2 negative with high proliferative index associated with malignant transformation [1,4,8].
It has been reported that higher expressions of P53 and Ki-67 have been related to worse prognosis, as well as large tumor size and greater proportion of the myoepithelial component rather than the epithelial one [2].
In our case, a suspicious nodule was found in a routine mammographic exam. Breast US and MRI imaging techniques were used to complete the diagnosis, confirming a nodule less than 1 centimeter with significantly increased vascularization and diffusion restriction at dynamic tests. Histological analysis was key for the diagnosis, showing the characteristic dual proliferation of epithelial and myoepithelial cells. Cellular atypia and mitosis figures were described, according to the literature, and Ki67 proliferation index was high, also as expected.
Differential diagnosis of AMEB should be made with intraductal papilloma with myoepithelial hyperplasia, sclerosing adenosis, fibroadenoma, adenoma, tubular carcinoma, adenoid cystic carcinoma, low-grade adenosquamous carcinoma, metaplastic carcinoma, malignant myoepithelioma, and papillary carcinoma [3,8].
Surgical treatment
Despite the lack of standardized management guidelines for MAMEB, according to the literature it is recommended to perform a complete excision of the lesion at an early stage with clear negative margins [1,2,4-6,8]. Some authors recommend a simple mastectomy, and although breast-conserving surgeries have been described with favorable outcomes, some authors suggest that insufficient excision or narrow surgical margins are associated to higher local recurrence rates [3,5,8]. In the presented case, a recurrence was observed 22 months after surgery, with surgical margins of 2 mm. Such margins are considered safe in case of ductal breast carcinoma but might not be enough according to some authors in cases of unusual tumors as MAMEB.
Wang et al. [4] recently described two case reports of a 34-year-old and 45-year-old patient with the diagnosis of MAMEB, both treated with breast conserving surgery (lumpectomy). Both women received chemotherapy and radiation therapy after surgery. No recurrencies have been described in neither of them so far [4]. Similarly, in a case report by Parikh et al. [1], a lumpectomy was performed in a 61-year-old patient with MAMEB who refused adjuvant therapy, with no recurrences to date [1].
On the other hand, there is controversy regarding the need to assess lymph nodes status, with significant heterogeneity between studies. According to low rates of lymph node invasion reported in literature, MAMEB is thought to spread through hematogenous rather than lymphatic pathway [2,5,8]; therefore, axillary staging by sentinel lymph node biopsy would not be recommended.
Regarding initial tumor size in this specific case, lumpectomy was proposed as the first surgical approach, resulting in negative margins at final pathological specimen. During the follow up, an image suspicion of local recurrence was assessed by biopsy, but pathologist could not confirm a MAMEB recurrence. The case was discussed in the tumor board and individualized, proposing a diagnostic-excisional surgery. Due to the non-confirmation of the recurrence in the initial biopsy, a new conservative breast surgery was recommended to be performed as a surgical biopsy since the ratio volume to excise vs breast volume was favorable.
Adjuvant treatments
Adjuvant treatments such as chemotherapy and radiotherapy for MAMEB have been performed in some cases, but the benefit for these cases remain under discussion [1,2,4,6,8]. Usually, when the MAMEB has a clear epithelial transformation like a carcinoma, these cases should be managed in accordance with standard breast cancer protocols.
In this specific case, due to scarce evidence reported in the literature regarding MAMEB, the Tumor Board agreed to not provide further adjuvant treatments neither axillary staging, but it was pointed to consider radiation therapy in case of a second recurrence.
Conclusion
MAMEB is an unusual type of breast cancer, and diagnosis is one of its main challenges, usually presenting nonspecific features on conventional imaging. Immunohistochemistry plays a key role in its differentiation when assessing its pathology. No standardized treatment has been established due to the exceptionality of MAMEB. However the basis of its management relies on the complete surgical excision of the lesion with safe margins, being possible the conservative surgery management according to the literature; although insufficient excision or narrow surgical margins are the main factors linked to higher recurrence rates. The role of MRI in staging may be important for guiding subsequent excision.
There is not enough evidence to support neither axillary lymph node systematic analysis nor adjuvant radiation or chemotherapy treatment in these patients. Nevertheless, a wide variation of treatments can be found in literature, with no clear consensus on the best therapeutic option.
Although this neoplasm accounts for a minimal proportion of breast cancers, it can have an aggressive behavior and quickly compromise patients’ life expectancy and quality of life. Thus, it is essential to gather more quality evidence regarding MAMEB to optimize the management of these patients.
Funding
None.
Conflict of interest statement
The authors declare having no conflicts of interest.
Ethical review of the case
This case report adheres to the law of Data Protection and was conducted ethically in accordance with the World Medical Association Declaration of Helsinki. The patient provided written informed consent to use her data.