Introduction
Maternal re-admission after childbirth is considered an indicator of the maternal morbidity and quality of care provided by healthcare. This significantly affects the mother-infant bonding and adds to the cost of maternity care. Several studies [1-5] have been undertaken to identify reasons and risk factors for maternal re-admission and various recommendations have been proposed. They have also noted an increase in rates of re-admission over the years.
The National Maternity and Perinatal Audit (NMPA) [6] is led by the Royal College of Obstetricians and Gynaecologists (RCOG) in partnership with the Royal College of Midwives (RCM), the Royal College of Paediatrics and Child Health (RCPCH) and the London School of Hygiene and Tropical Medicine (LSHTM). The NMPA is commissioned by the Healthcare Quality Improvement Partnership (HQIP) as part of the National Clinical Audit and Patient Outcomes Programme (NCAPOP) on behalf of the National Health Service (NHS) England and the Welsh Government. According to the report from the NMPA, the rate of maternal postnatal re-admission is 3.3% across England & Wales, with more women re-admitted after caesarean (4.3%) than vaginal birth (2.9%).
These figures are based on births in maternities of the NHS in England and Wales between 1 April 2018 and 31 March 2019. The recommendations were to review all cases of postnatal maternal re-admissions to understand common indications and identify changes in practice that may decrease the chances of re-admission, especially among those having a caesarean birth.
Methods
We performed an audit to understand the reasons for maternal re-admission, thereby identify ways to reduce the re-admission rate in our hospital. The standards for this audit were obtained from the NMPA clinical report published in 2022 and also a previous audit conducted in our hospital.
This was a retrospective study, conducted at Basildon university hospital. This is a medium sized District General hospital in the East of England. Women who were re-admitted within 42 days after childbirth between January and December 2022 were studied. This data was obtained from DATIX, which is our risk management information system. The information of women who are re-admitted within 42 days of giving birth is submitted onto our DATIX system. Women who were admitted exclusively to care for their baby who were under treatment, were excluded from our study.
The case notes were reviewed from our electronic records. The following information were collected: reason for re-admission, duration of re-admission, received treatment, any surgeries performed, time of consultant review, follow up plan for hypertension management. The results were analysed and compared with the results of the previous audit.
A similar audit was conducted in our hospital between January- August 2020. The recommendations from this audit were to perform an audit on wound infections, create postnatal blood pressure (BP) follow up plans for women on anti-hypertensives at discharge as recommended by The National Institute for Health and Care Excellence (NICE) [7]. Women with raised BP are followed by community midwives. They have BP checked between postnatal day 3 and day 5. They are then advised to follow up at primary care for hypertension management from 2 weeks postpartum. Some women with severe pre-eclampsia have individualised follow up plan.
Results
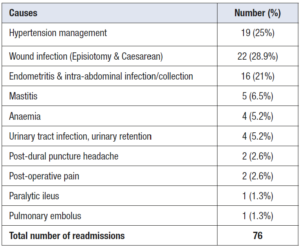
The number of women needing re-admission within 42 days (puerperal period) of giving birth/ pregnancy loss were 76. The number of births for the same period of year January-December 2022 was 3,773 including late miscarriages. This excludes the early pregnancy losses. The rate of re-admission was 2% in this study. The rate of re-admission from the NMPA clinical report suggests 3.3% overall rate in England. The average duration of stay at hospital was 4.0 days (2-18 days).
Totally 60 (79%) women were reviewed by consultant during their hospital stay. 38% of women were reviewed by consultant within 14 hours. 21% were not seen by consultant during their hospital stay. Our hospital policy recommends patients to be reviewed by a consultant within 14 hours of their admission, to improve the provided quality of care. This is also one of the standards set by NHS England - Seven Day Services Clinical standards [8]. As per these standards, all emergency admissions must be seen and have a thorough clinical assessment by a suitable consultant as soon as possible but at the latest within 14 hours from the time of admission to hospital. But this target is not achievable 100% as the consultants are not in the hospital round the clock especially over the weekend and after 20:00 hours over weekdays. (Table 1)
Raised Blood Pressure (BP)
19/76 (25%) women were re-admitted for hypertension management. 8/19 of these women were known to have pre-eclampsia/hypertension. 7/8 (87%) of these women had follow up plans made for BP monitoring previous to discharge following birth. 7 of the women admitted for hypertension control were not known to have hypertension/ pre-eclampsia during the antenatal/ intrapartum period. 4 women had delivered in other hospitals and hence we could not access data of their postnatal follow up plans.
Infection
16 women were admitted with endometritis/ intra-abdominal collection post birth. They were all successfully managed with parenteral antibiotics. Of them, one woman needed admission to Intensive Care Unit for management of severe sepsis.
Wound infection
22/76 (28.9%) women were admitted for management of wound infection. Of them, 4 had episiotomy infection and 18 had infection of the caesarean wound. The four women readmitted after vaginal deliver needed parenteral antibiotics and one patient needed evacuation of a vaginal haematoma and re suturing; however, all cases showed good response to therapy. Of the 18 women readmitted after caesarean section, 2 of them underwent a second surgery to clean and re-suture the wound.
Other complaints
Four women were admitted with symptomatic anaemia, all of them received blood transfusion. Some of them had declined transfusion initially post birth and were re-admitted as they became more symptomatic. Two women were re-admitted for epidural blood patch following post-dural puncture headache. Two women were admitted with poorly controlled post-operative pain. One woman had paralytic ileus which resolved with expectant management. One woman was admitted with chest symptoms and found to have pulmonary embolus. She had a history of recurrent deep venous thrombosis (DVT) and was on therapeutic enoxaparin, she was later transferred to a medical team.
Previous audit
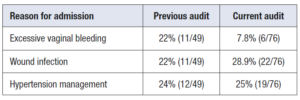
This was a retrospective audit on postnatal maternal re-admissions undertaken in our hospital. They found 49 women were admitted between January- August 2020. 11/49 (22%) were admitted with heavy vaginal bleeding. 6 of them had surgical evacuation of retained products. 11/49 (22%) were admitted with wound infection. 12/49 (24%) were admitted for BP management. They found women did not have a clear plan to monitor BP in the community. The recommendations were to make clear plans for follow up of women with raised BP upon discharge. The other reasons for re-admission were mastitis, abdominal pain, suspected DVT and persistent headache needing evaluation. A plan was made to perform a detailed audit on wound infection but unfortunately this has not been undertaken yet. (Table 2)
Discussion
Maternal re-admission after birth is a maternity morbidity indicator. Girsen et al. [9] reviewed the rate and causes of severe maternal morbidity at readmission in California. In their study, 1% of women were re-admitted and 17.3% of these women had severe maternal morbidity. Re-admission can be due to multiple causes some of them are preventable.
Readmission can affect the maternal/neonatal bonding, breastfeeding, and leads to anxiety in family. It also adds to the cost of maternity care, increases bed occupancy, affects the patient flow from delivery suite to postnatal ward. It adds to workload for the already overworked staff. The duration of stay at a hospital following birth has decreased over the years. The maternity survey of 2023 [10] shows peoples’ experience of care has deteriorated over the last 5 years. Only 55% of women were able to get a member of staff to help when they needed after birth. The shortage of midwifery and support workers affects the quality of care provided for postnatal mothers. A study has shown women in trusts with more midwifery staff have reported better postnatal experience [11].
Bowers et al. [12] have estimated the cost of routine postnatal maternity care while being in patient per woman at 692 pounds for 36 hours. We can expect the cost to be higher when they need additional investigations, treatment, and intensive care. They also suggest longer hospital stay for women with higher acuity mothers. This can reduce the demand on community postnatal care. Women with high risk factors are at increased risk of re-admission after birth. Identifying these women can allow us to make specific plans for postnatal follow up. Women can be made aware of symptoms and signs of complications, to review earlier to get timely help.
In our audit, a total of 19 women were readmitted due to hypertensive disorders after childbearing. On comparing with our previous audit, the rates of re-admission for hypertension management remained similar. Studies have shown women with risk factors are highly likely to be re-admitted for hypertension management [13]. In a retrospective study by Bruce et al. [1], re-admission rate for hypertension management was 4.43% amongst women known to have hypertensive disorders of pregnancy. Women with increasing maternal age, severe antepartum hypertension, and persistent postpartum BP ≥1 40/90 were more likely to be re-admitted. Another retrospective study by Lovgren et al. [14] has shown higher risk of re-admission if systolic BP was ≥ 140 and diastolic BP was ≥ 90 mm Hg prior to discharge from the hospital. In our audit we had not reviewed if target BP was achieved prior to discharge after birth. Hence, we have added this to our recommendations to aim for 135/85 mmHg for at least 24 hours prior to discharge.
Among the 16 women readmitted with severe infectious processes after deliver those who need long term parenteral antibiotics were managed by the ‘Hospital at home’ team with guidance from the Microbiology service. Once the women were clinically stable to be discharged, included the one who need intensive care, they had a peripherally central catheter line inserted. The community nurse visited these women at home, performed observations, blood tests as needed, and administered parenteral antibiotics. This practice reduces the duration of stay at the hospital, allowing them to be with their family.
The previous audit identified more women re-admitted with more than expected vaginal bleeding, half of them (6/11) had surgical evacuation of retained products. There was departmental teaching on management of endometritis/ retained products. In our current audit we did not have any woman who needed surgical evacuation of retained tissue.
Wound infection
A total of 22 women needed to be readmitted in the postpartum period due to wound infection. On comparing with our previous audit, the rate of re-admission for wound infection has increased from 22% to 28.9%. This could be attributed to an increase in caesarean rates over the years. Our audit captured only the women who needed re-admission with wound infection. This does not include women who were managed as outpatient. Hence, it may not capture the total number of women with wound infections. Hence a more detailed audit on wound infection is recommended to identify any factors that could reduce wound infection rates.
In an audit on re-admissions following caesarean at the Irish Maternity hospital, Panda et al. [15] showed infection or suspected sepsis as the commonest reason for re-admission. The majority of them were treated with analgesics and parenteral antibiotics. Rate of re-admissions and duration of stay were higher amongst women who had emergency caesarean than an elective caesarean procedure. The second most common cause for re-admission was hypertension. The average stay at hospital during re-admission was 2.6-4.6 days.
Surgical site infections (SSI) are one of the commonest morbidities following a caesarean section. A 3-18% of women can develop SSI post caesarean [16-20]. Women with certain risk factors are found to have higher incidence of SSI. A meta-analysis by Zhu et al. [21] found smoking, previous caesarean delivery, multiple vaginal examinations in labour, premature rupture of membranes, hypertensive disorders, diabetes mellitus, obesity as correlated risk factors for SSI following a caesarean section. Several studies [22,23] have looked at various ways to reduce SSI, such as prophylactic antibiotics, vaginal cleansing prior to caesarean section, surgical techniques, special dressing and so on. The NICE has previously published the guidelines for SSI: prevention and treatment [24] and caesarean birth [25]. Some of their recommendations are appropriate prophylactic antibiotic prior to skin incision, use of hair clippers only if needed, controlled cord traction for placental delivery, avoid closure of the subcutaneous space unless more than 2 cm in depth, avoid superficial drains and staples for skin closure.
One of the limitations of our audit is that we did not look in detail the risk factors for women with infectious morbidity. Since the number of women re-admitted with infections has risen when compared to the previous audit, we recommend a separate audit on women with wound infections and endometritis. This can look at risk factors for infections and review our practice to identify ways to reduce the morbidity from infections.
Recommendations from our study
Only 38% of women were seen by consultant within the set target of 14 hours. This can be improved by mentioning about these admissions at the morning and evening handover in the delivery suite. We also noted incomplete documentation; hence we emphasize on clear documentation of when and who reviewed the women.
To reduce the rates of re-admission for hypertension management, we recommend achieving a target BP of <135/85 mmHg for at least 24 hours before discharge after birth, and perform future audits to review if this target can be met.
To undertake a detailed audit on rates of wound infection, to identify any risk factors, to review antibiotic therapy and propose any strategies to reduce the rate of infection based on available evidence.
We also recommended to re-audit maternal postnatal re-admissions on a yearly basis.
Conclusion
Our study showed a maternal postnatal re-admission rate of 2% in our hospital. This is less than the rate for England. We cannot prevent all re-admissions. As postnatal period is a crucial time for family bonding with the new-born, we should aim to reduce avoidable re-admissions. This shall improve patient satisfaction and reduce healthcare cost.
Conflicts of interest
None.
Funding
No financial relationships to disclose