Introduction
Pelvic organ prolapse (POP) is a condition that affects many women and is detrimental to their everyday activities, sexual function and quality of life. The etiology of POP is complex and includes several risk factors such as vaginal childbirth, advancing age and increased body mass index. Some studies have also shown a genetic or hereditary component to the disorder [1,2].
Available treatments for POP include conservative – aimed at prevention or symptom management, or surgical – which aim to repair and strengthen the tissues that support the prolapse. The most often prescribed conservative treatment option is the use of vaginal pessaries, which are inserted into the vagina to provide support to the prolapsed tissue. Although this approach can help by easing symptoms, it has been connected with low rates of long-term patient compliance [3].
Surgical approaches for POP rely on tissue reconstruction either by a native tissue suture application or by tissue repairs augmented with permanent synthetic mesh or a biological graft [4], either via the transvaginal or abdominal route.
In recent years, surgical management of POP has been under increased scrutiny due to frequent complications and adverse events following tissue repair using synthetic polypropylene meshes. As a result, patients are now more reluctant than ever to have surgery for their prolapse [5-8].
For the reasons stated above, there is an urgent need for new non-surgical therapies for POP. A promising approach in recent years has been the introduction of vaginal erbium laser (VEL) treatment for POP [9-12]. Non-ablative VEL treatment with SMOOTH® mode utilizes thermal pulsing to elevate the temperature of the upper mucosal layers and strengthen the vaginal wall's connective tissue that supports the prolapse, as well as the whole vaginal canal [13,14]. It has been shown to improve the tissue quality and to alleviate the symptoms of various disorders that arise from pelvic floor dysfunction, including stress urinary incontinence (SUI) and POP [9-19].
POP and SUI frequently coexist [20]. Similar to prolapse, SUI therapies can be either conservative, mainly including some form of pelvic floor muscle therapy, or surgical, in most cases consisting of mid-urethral synthetic sling insertion. Although conservative approaches have shown to be effective, they suffer from low patient compliance. Schiøtz et al. have shown that 10 years after initiating conservative therapy, 85% of patients discontinued the treatment [21].
We have been using the VEL in our practice since 2013 with very good outcomes in women with cystoceles as well as SUI. The aim of the present retrospective study was to analyze patient data from our clinical practice to objectively assess the effectiveness of non-ablative VEL for the treatment of patients with cystocele and co-existing SUI, if present.
Materials and methods
Laser treatment
All the included patients received a non-ablative Er:YAG treatment for POP – ProlapLase® (Fotona, Slovenia). The laser procedure consisted of Er:YAG laser irradiation of the whole vaginal canal with SMOOTH® mode, followed by additional irradiation of the prolapsed anterior vaginal wall (and posterior wall, if a rectocele was present). The procedure was concluded with irradiation of the vestibule and introitus area. Depending on the prolapse severity, multiple passes of laser irradiation were applied, with emphasis on the irradiation of the prolapsed portion of the vaginal wall. Around 1500 J of laser energy were delivered to the vaginal mucosa per session. The procedure has been explained in detail in a study by Bizjak-Ogrinc et al. [10]. The procedures were performed in an ambulatory setting, without anesthesia or post-treatment medications. The treatment time was approximately 30 minutes. Most patients received several laser sessions, with 4-6 weeks intervals between consecutive sessions.
Data collection and analysis
This study was a retrospective analysis of data recorded from patient charts. The study was conducted according to the principles of the Helsinki Declaration and the Oviedo Convention on Human Rights and Biomedicine and received an Ethics Committee approval. Informed consent was signed by all patients. All patients with POP treated with ProlapLase® were included into the study. Collected demographic parameters at baseline included age, parity and mode of deliveries.
The POP grade was based on the Baden-Walker scale which was recorded at baseline and at every session [22]. The location of the prolapse (cystocele, rectocele or both) and the potential coexistence of SUI were recorded as well. In a limited number of patients, before and after photographs of the cystoceles were taken under strain. SUI was assessed at baseline and at each follow-up using the International Consultation on Incontinence Questionnaire (ICIQ-UI) short form questionnaire. The ICIQ-UI short form score was calculated from Questions 3, 4 and 5 of the ICIQ-UI standardized questionnaire [23].
Patient satisfaction was assessed at every follow-up using a satisfaction questionnaire in which women graded their satisfaction on a scale from 0 (most unsatisfied) to 10 (most satisfied). Adverse events were also recorded. All collected parameters were included into an anonymized data sheet. Statistical data analysis was performed using Prism software (GraphPad, USA).
Results
From 2015 to 2016 a total of 41 patients with cystocele were identified and treated in our clinic using ProlapLase®. Of these, 27 also presented with coexisting SUI. When representing the results, the term Group A was used to represent the group of all cystocele patients, and the term Group B to represent only the subgroup of the 27 cystocele patients that had coexisting SUI.
The average age of patients in Group A was 51 (CI: 46.7-55.2), while in group B it was 52 (CI: 46.5-57.5). Both groups had 1.9 deliveries on average (CI: 1.8-2), with each group having mostly vaginal deliveries and only 1 patient had 1 cesarean section and 1 vaginal delivery. There were no significant differences in age or parity between the two groups.
All 41 patients were diagnosed with cystoceles upon vaginal examination; 2 patients also presented a rectocele. Patients with a rectocele received a posterior vaginal wall treatment in additional to a whole vaginal canal and anterior vaginal wall laser treatment.
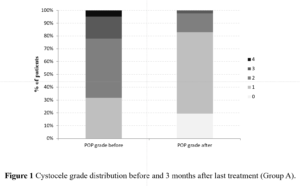
The average cystocele grade in Group A was 2, while in Group B it was 1.96. The patients received between 1 and 5 treatment sessions, with 2.7 laser sessions on average. The interval between sessions was 4-6 weeks. The average cystocele grade after the final treatment session was 1 in both Groups. There was no statistical difference between groups in cystocele stage before or after treatment sessions. The cystocele grades decreased by 0.95 on average (Table 1 and Figure 1).
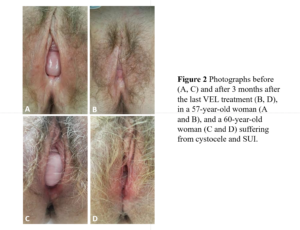
Figure 2 depicts before and after images from two patients. Photographs were made under abdominal strain and were taken before and after a completed series of treatments (Figure 2).
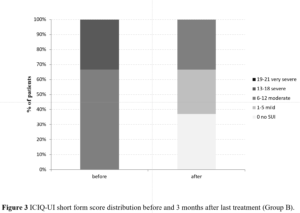
In Group B, SUI was also evaluated using the ICIQ-UI questionnaire before the first treatment session and 3 months following the last received session. The average ICIQ-UI score at baseline was 11.33, which decreased to 3.56 after the completed treatment sessions. The ICIQ-UI score improved by 7.78 points, on average. At baseline, out of 27 patients in Group B, none were dry or with mild symptoms, 18 (67%) had moderate symptoms of SUI, 9 (33%) had severe symptoms, while none had very severe symptoms. Three months after the last received treatment, 10 patients (37%) of group B were dry (ICIQ-UI SF score = 0), 8 (29.6%) only had mild symptoms, while 9 (33.3%) had moderate symptoms of SUI (Table 2 and Figure 3); 26 patients (96.3%) had improved their ICIQ-UI short form score, one patient's score was the same as at baseline and none of the patients had worsened.
Patient satisfaction on a scale from 0-10 was measured after the first treatment and after the last series of treatments. The satisfaction after the last visit was significantly higher (p<0.001) than after the first visit, 6.37 vs. 8.81, respectively, indicating an increase of patient satisfaction with time and additional treatment sessions (Table 1). There were no reported adverse events among the patients.
Discussion
Our retrospective study has shown that treatment with ProlapLase® was effective in managing cystoceles and concomitant SUI. The patient satisfaction rate with the treatment was high and the treatment had an excellent safety profile. To our knowledge, this is the first study which has shown the improvement of both POP and SUI symptoms after non-ablative VEL treatment in patients suffering from both conditions.
Non-ablative VEL treatment for POP is one of the newest treatments available for this condition. It has been introduced to clinical practice only in the last few years, with the first clinical cases reported almost a decade ago13. Non-ablative Er:YAG laser with SMOOTH® mode is safe to be used inside the vaginal canal, as the laser pulses achieve controlled heating of the collagen in the layers of the mucosa up to the lamina propria, without ablating or damaging the mucosal surface. Therefore, there is no risk of damaging underlying structures, such as the urethra, bladder, or rectum.
It works by quick heat-pulsing of the vaginal mucosa, increasing the temperature of the tissue up to 65 degrees in short pulses [14,24,25]. The result of this is collagen contraction and the stimulation of new collagen formation and stimulation of tissue regeneration via activation of paracrine signaling pathways, with the combination of both effects resulting in functional strengthening of the vaginal wall and improved tissue quality.
Lapii et al. [26] have shown that the volume density of blood capillaries and the thickness of the epithelial layer increased by 61.1% and 64.5%, respectively, following vaginal non-ablative laser treatment.
Gaspar et al. [27] and Bezmenko et al. [28] have also shown that significant morphological changes occur in vaginal mucosa post Er:YAG SMOOTH® treatments.
The ultimate result of vaginal erbium SMOOTH® treatments is better pelvic floor support, which helps alleviate or diminish the symptoms of pelvic floor disorders. The Integral theory of Petros [29] emphasizes the important role of vaginal wall laxity in pelvic floor dysfunction symptoms. Indeed, the non-ablative laser treatments, which effectively strengthen the vaginal wall, have shown to be effective in alleviating many symptoms of pelvic floor dysfunction, including SUI [16-18,30-34], vaginal laxity [15,19], and POP [9,10].
Our study has shown improvement in cystocele grades in 36 out of 41 treated patients (87.8%). Most of the patients (28 of 41, 68.3%) had a level 2 or higher grade of prolapse at baseline. After the completed series of treatment sessions, only 7 patients (17.1%) had a level 2 or higher grade of cystocele, while all the other patients were grade 1 (n=26) or 0 (no cystocele, n=8). Interestingly, all 5 patients that did not show improvement had a mild, grade 1 cystocele at baseline, while the highest improvement (by 2 grades) was evident in 2 patients with grade 3 cystocele and one patient with grade 4 cystocele. Our data corroborates the results of Ogrinc et al. [10], who have seen improvement by 1.6 grades of cystocele according to the same scale used in our study, with the improvement being highest in the patients that had more severe symptoms. The Ogrinc et al. study had a higher proportion of patients with prolapse grade 3 or higher at baseline (34% vs 19% in our retrospective study). The results of this data together indicate that even patients with more severe symptoms could benefit from this minimally invasive treatment, suggesting that the standard offering of this treatment to all prolapse patients prior to surgical intervention should be considered. Our data is not in concordance with a study published by Athanasiou et al. [35], who found no significant difference in POP symptoms between the Er:YAG vaginal laser treatment and a sham. However, the Athanasiou et al. study had a short follow-up time, it included an older cohort with median age of 67 (in our study median age was 51) and was not limited to cystocele treatment – all these factors probably having a negative influence on the results of the laser treatment.
In our study, of 41 patients, 27 (65.9%) had a coexisting SUI. This proportion of coexisting SUI is consistent with that previously reported in the literature [20]. All but one patient (96.3%) reported improvement in their SUI symptoms. The average improvement was 7.78 points on the ICIQ-UI short form scale, which was statistically significant and also much higher than the minimal values of clinically meaningful improvement that has been previously reported in literature, ranging from 2.5 to 4 points [36,37]. Interestingly, out of 5 patients that had not improved in cystocele grade after the treatment, 3 had a coexisting SUI – of these 3, all had significantly improved their SUI symptoms, with an average ICIQ-UI SF grade decrease of 9.33 and an average satisfaction of rate 9.67 out of 10. The improvement in incontinence measured by the ICIQ-UI short form score is comparable to that reported in previously published studies regarding non-ablative Er:YAG vaginal treatment for SUI, which ranged from a decrease of 3.86 points after a single treatment [17] to a decrease of more than 10 points [30] in the ICIQ-UI short form score after three treatments. These data, along with a new study published by Kuszka et al. [18], indicate that the effectiveness of non-ablative Er:YAG laser for treating SUI increases with an increased number of sessions.
Our study shows a unique benefit of non-ablative laser treatment for women who suffer from both cystocele and SUI. Usually when these women opt for surgical management of POP and SUI, they require two operative procedures, one for each condition, increasing their overall risk of adverse events [38].
Non-ablative VEL can treat both conditions at once, and there are indications that a relief of symptoms may occur even in the higher grades of POP. However, more clinical trials with higher grade of medical evidence are needed to confirm our assumptions.
There has been a lot of controversy since the US FDA issued a letter to 7 companies in 2018, warning against the advertising of energy-based devices, including lasers, for vaginal treatments; indeed, to date, none of these devices have been approved for use in the United States. However, non-ablative VEL has been clinically approved for sale and has been in clinical use in Europe and many other countries for SUI since 2012 and for POP since 2017. The FDA warning letter has motivated the largest post-marketing clinical follow-up study of vaginal erbium treatments thus far, which has gathered data from more than 113,000 patients worldwide and has confirmed the excellent safety profile of this technology [39].
Our study has corroborated this safety profile, as there were no reported adverse events among the 41 treated patients.
Conclusion
This retrospective study has shown that non-ablative Er:YAG laser treatment with SMOOTH® mode seems to be an effective and safe option for reducing the grade of cystocele as well as symptoms of coexisting SUI.