Introduction
Infertility is a common reproductive health problem defined as the inability of a couple to conceive after 12 months of sexual intercourse without contraception, or limited reproduction individually or with a partner [1]. It affects approximately 15% of couples of reproductive age [2, 3]. The etiology of infertility is multifactorial, but in one third of cases it is caused by a female factor [4]. Tubal pathology is a common cause of female infertility, representing about 30-35% of infertility among women of childbearing age, making the assessment of tubal patency a fundamental step in the workup of infertile couples that should be prioritized [5,6].
An ideal imaging technique for evaluating infertility should be noninvasive, inexpensive, quick and easy to perform, and at the same time provide information on both pelvic disorders and tubal patency. In the past few years, Saline Infusion Sonosalpingography (SIS) has become the first-line diagnostic test to assess tubal patency, replacing hysterosalpingography (HSG) [7,8], being a quicker, cheaper and easier to perform method. It is an ultrasound-based imaging technique that involves the introduction of saline solution (or saline mixed with air) [9] into the uterine cavity and fallopian tubes allowing an accurate evaluation of tubal conditions, through a dynamic acquisition of real time images. The use of air and saline medium makes it even more simple and inexpensive without affecting the results, and the absence of radiation or irritant contrasts implies improved comfort, patient compliance and pain scores [9]. Moreover, it has been proved that it has the same accuracy in evaluating the patency of fallopian tubes compared with laparoscopy or HSG [10,11]. However, it requires a well-trained sonographer with experience in the procedure and patience, in order to determine how to differentiate between a real occlusion and a temporary spasm [12].
There are several studies assessing the possibility of tubal patency tests, including SIS, to promote a spontaneous pregnancy [8,13,14]. Furthermore, studies have suggested that pregnancy rates (PR) could be directly increased in the months following these procedures, as well as a fertility-enhancing effect with higher rates of ongoing pregnancy showed by a meta-analysis by Chunyan et al. [13] regarding hysterosalpingo-contrast sonography. Various theories have been proposed, namely, that the passage of fluid may release small obstructions through the fallopian tubes [13,14] or that these interventions may improve endometrial perfusion [15] or even play a role in inducing ovulation [4].
Accordingly, it has been suggested that some couples may benefit from expectant management in order to reduce overtreatment and waste of medical resources. However, clinical characteristics of couples most likely to benefit from expectant management or for how long are not yet well understood. Thus, the aim of this study was to identify the predictive factors for spontaneous conception following SIS.
Methods
Study population and design
We performed a retrospective cohort study including women who underwent SIS between January 2017 to December 2020 at a Reproductive Medicine Unit of a tertiary University Hospital in Portugal.
A total of 704 patients who underwent SIS in this period were selected, of which 468 were eligible for the study. Exclusion criteria were: severe male infertility (less than eight million sperm/mL with normal morphology after migration), and assisted reproduction treatment (ovulation induction, intrauterine infusion or in vitro fertilization) between SIS and conception.
The main outcome of this study was spontaneous pregnancy within the 12 months following SIS. Accordingly, patients were divided in two groups: pregnancy after SIS (n=75) and non-pregnant (n=373). The following clinical characteristics were evaluated as potential predictive factors: age, body mass index (BMI), duration and primary infertility cause, obstetric history, characteristics of menstrual cycles, smoking habit, pelvic and uterine surgical history, ovarian reserve [anti-Mullerian hormone (AMH) and antral follicle count (AFC)], SIS report (bilateral tubal occlusion, unilateral tubal occlusion or patent tubes) and semen parameters (sperm concentration, motility and morphology) of which normal cut-off values were based on World Health Organization (WHO) 2010 criteria. Secondary outcomes included: time to conception, live-birth and miscarriage and ectopic pregnancy.
The research was performed according to the Declaration of Helsinki of the World Medical Association. The approval of Institutional Review Board was waived since the anonymity of all the patients was guaranteed and due to the retrospective study design, which did not involve experiments with humans neither any change in clinical conduct or follow-up.
Saline Infusion Sonosalpingography (SIS)
SIS was performed until the 12th day of menstruation. Patients were asked to empty their bladder, placed in lithotomy position and the cervix was routinely disinfected with a povidone-iodine solution. An intrauterine catheter was inserted into the uterine cavity through the cervical canal and connected to a pre-warmed saline infusion system.
A two-dimensional transvaginal ultrasound was performed previously to evaluate the uterus and adnexa and exclude contraindications to the procedure (hydrosalpinx, ovarian tumor, corpus luteum). Tubal patency was defined by visualization of passage of air or fluid through the fallopian tubes to the ovary, or the visible fluid spill from the fimbriae to the peritoneal cavity through ultrasound using the transvaginal probe [16].
According to tubal patency, patients were divided into 3 categories: type 1, defined as bilateral tubal occlusion; type 2, defined as unilateral tubal occlusion; and type 3, defined as normal patent tubes.
All ultrasound examinations and evaluation reports were carried by four sonographers, each of whom had more than five years of experience in performing gynecologic and obstetric ultrasound examinations. A Voluson E8 Expert (GE Healthcare, Zipf, Austria) with an RIC5-9-D transvaginal volume transducer with a frequency range of 5.0–9.0 MHz RIC5–9-D volume probe (5–9 MHz) was used.
Statistical analysis
Statistical analysis was performed using SPSS® version 26.0. The normality of distributions was assessed using the Shapiro-Wilk test. Categorical variables are presented as number of cases and percentages (%) and continuous variables as mean ± standard deviations when they followed a normal distribution, and median and minimum and maximum values (range) when they did not. Differences between two independent variables were assessed using the Student-T test for independent variables or the Mann-Whitney U test, according to the normality of distribution of the variables. The comparison of two or more categorical variables was performed using the chi-square test (χ2). Pearson's test was used to assess the correlation of factors with time of conception. Kaplan–Meier was used to calculate cumulative incidences of pregnancy and time to conception after SIS. Logistic regression analysis was performed to identify variables correlated with spontaneous pregnancy. A p value <0.05 was considered as statistically significant.
Results
A total of 75 infertile women (16%) conceived within 12 months after SIS. The comparison of clinical characteristics between pregnant and non-pregnant groups is shown in Table 1. Median age of the group of women who became pregnant was 34.0 years versus 35.0 years in those who did not become pregnant (p=0.013). In the group of women who did not become pregnant, 21.4% were obese versus 12% in the pregnant group (p=0.030).
The mean time of infertility was 2.7 ± 2.1 years for those who did not become pregnant versus 1.9 ± 0.9 for those who became pregnant (p<0.0001). Regarding the markers of ovarian reserve, median AMH was 1.8 ng/mL in the non-pregnant group versus 2.4 ng/mL in the pregnant group (p=0.002), and the median AFC was 10 in the non-pregnant group versus 12 in the pregnant group (p=0.03).
No significant difference was observed in the primary infertility cause, obstetric history, previous pelvic or uterine surgery, history of chlamydial infection, smoking habit and menstrual cycles between the two groups. Median age of the partner in the group that did not get pregnant was 36 years vs 35 years in the group who became pregnant (p=0.019) and there were no statistical differences regarding semen characteristics (Table 2).
The cumulative rate of spontaneous pregnancy during the 12 months after SIS was 16%. The mean time to conception was 3.4 ± 2.9 months (range 0.5-6.3). The PR was significantly higher in the first 30 days after SIS (33.3%) compared to the other months of observation (p<0.0001) (Figure 1).
The PR at 1-3 months, 1-6 months, 1-9 months and 1-12 months was 10.5%, 13.5%, 15.6% and 16.0%, respectively. At 1–3 months, 4–6 months, 7–9 months and 10–12 months accounted for 65.3%, 18.7%, 13.3% and 2.7% of the total cumulative PR, correspondingly.
During the study period, 64 (13.4%) of the patients had bilateral tubal occlusion (type 1 category), 143 (30%) had unilateral tubal occlusion (type 2 category) and 261 (54.7%) had patent tubes (type 3 category). Within a year after SIS, the incidence of spontaneous pregnancy was 18.4% (n=48) in type 3, followed by type 2 with 13.3% (n=19) and type 1 with 12.5% (n=8) (p=0.290) (Figure 2).
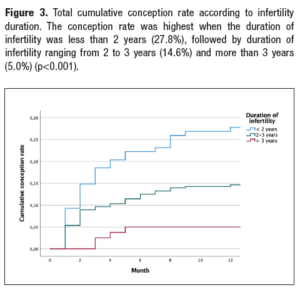
The PR was highest among women who were infertile for less than 2 years (27.8%), followed by duration of infertility ranging 2 to 3 years (14.6%) and the duration of infertility more than or equal to 3 years (5.0%) (p<0.001) (Figure 3).
Logistic regression analysis showed that AMH was the only independent variable capable of influencing the incidence of pregnancy between the two groups (odds ratio [OR] 1.47 95% CI: 1.11, 1.67; p=0.002).
Regarding obstetrical outcomes, 84% (n=63) of the pregnant women had a live birth, 9.3% (n=7) had a miscarriage and 4% (n=3) had an ectopic pregnancy; there were 2 cases lost to follow-up (2.7%).
Discussion
In our study, the pregnancy group was characterized by younger women with a higher percentage of normal weight, a shorter duration of infertility and higher functional ovarian reserve. Insights into predictive factors of spontaneous conception after SIS can help clinicians to elect patients for expectant management, which could reduce overtreatment and clinical risks associated with assisted reproductive techniques and, at the same time, save medical resources.
Our results indicate BMI as a predictive factor of pregnancy after SIS, which is in accordance with the negative impact of obesity on female fertility [4,17], contributing to anovulation and menstrual irregularities, reduced conception rate and response to fertility treatments and higher rated of miscarriage. In fact, in a study by Giuliano et al. [4]. BMI was the only variable that was able to determine the PR in the whole study, and was determinant even if within normal values.
Also, our findings suggest that shorter duration of infertility is strongly associated with spontaneous conception after SIS which is in agreement with previous studies [4, 5, 18]. This can be attributed to the long-term tubal obstruction causing chronic inflammatory reactions that can damage internal tubal structures [5,19].
Age was a predictive factor of spontaneous pregnancy, which is not surprising, due to the robust evidence demonstrating a lower chance to achieve pregnancy in women with advanced maternal age [4]. Nonetheless, AMH was the only variable explaining the difference in the incidence of pregnancy between the two groups, as demonstrated by our logistic regression analysis (odds ratio [OR], 1.47; p=0.002), which reinforces the value of AMH as a predictive factor of spontaneous pregnancy [4, 18].
In our study, we report a PR of 16%, which is comparable to one study [4]. However, there have been studies with higher PR, like 40.9% [5] or 26.59% [13], which can possibly be explained by the fact that Liu et al. [5] excluded infertile couples with semen abnormalities according to WHO 2010 guideline, and by the relatively large proportion of bilateral tubal patency (67.5% vs. 54.7%) and small proportion of bilateral tubal obstruction (9.5% vs. 13.4%) found in their study.
Such a high percentage of PR (16%) should not be considered accidental, and it is supported by the association of spontaneous pregnancy and the level of tubal patency, consistent with others studies where the level of fallopian tubes patency was significantly associated with spontaneous conception [4, 5, 13, 20]. Although in our study there were no statistical difference in PR according to the level of tubal patency, there was a tendency to higher PR in the group with bilateral patent tubes.
Several studies have reported the rate of spontaneous pregnancy in infertile women following these techniques. For instance, Wahby et al. [21], in 1966, reported a PR of 25% to 40% after HSG in couples with unexplained infertility; more recently, Nugent et al. [22] compared the PR in couples with instillation of an oil-soluble contrast media versus couples under no intervention, and reported a PR of 20% in the intervened couples versus no pregnancies in the other. Other studies have compared oil-soluble with water-soluble contrast media, although with controversy results [14, 15, 23]. Additionally, a Cochrane review of randomized trials confirmed that tubal flushing versus no intervention had relation to a significant increase in the odds of pregnancy and live birth [24, 25]. This positive effect may be explained by the action of the contrast agent in the way that the passage of liquid breaks up minor adhesion, removes debris and mucus plugs within the tubes caused by inflammatory processes and expands tubal stenosis and convolutions, that can negatively impact on fecundation [5, 13, 20, 24]. Nonetheless, other theories have been proposed, namely that these procedures could play a role in inducing ovulation [4] or improving endometrial perfusion [15], and hence its receptivity. In fact, Li et al. [26] demonstrated that endometrial blood flow distribution patterns showed significant changes after SIS, with these patients presenting improved endometrial blood distribution, which is associated with higher PR [26]. However, the underlying mechanism for this enhanced endometrial blood flow remains unclear; some theories have emerged, namely that the stress produced by the microbubble solution, together with the endometrial abrasion caused by the insertion of the catheter, might stimulate the secretion of cytokines and growth factors that support endometrium angiogenesis, thereby improving endometrial blood flow [26]. However, this is still a controversial topic [15, 27].
Conception was significantly higher in the first 30 days following SIS (33.3%), situation that has been previously reported in other studies [4, 13, 20]. This is compatible with the hypothesis of SIS favoring spontaneous pregnancy during the same menstrual cycle of the procedure [4, 24].
The mean time to conception in our study was 3.4 ± 2.9 months within a year after SIS, which was lower than that reported in other studies (8.8 ± 0.3) [5] and 5.3 [13]. This could mean that infertile couples might achieve spontaneous pregnancies within a short time after SIS and that an expectant management could be assumed for a certain period of time in order to reduce overtreatment, clinical risks and save medical resources.
Surprisingly, there were eight cases of spontaneous conception in women with type 1 SIS (bilateral obstruction), which has also been described in other studies [5, 13], probably due to the mechanic effect of the passage of liquid removing the buildup of debris inside it, to the false-positive results of tubal spasm during SIS [5] and to the theory that it is more difficult to diagnose tubal occlusion than tubal patency, which can lead also to some false-positive results [28].
Regarding obstetrical outcomes, the great majority of pregnancies resulted in a live birth (84%); there was 9.3% of miscarriages which is in line with the reported incidence of early pregnancy loss in clinically recognized pregnancies [29] and there were three cases (4%) of ectopic pregnancies, comparable to other studies reporting a prevalence of 1-2% [3] and to the incidence in the general population, suggesting that SIS did not increase the risk of ectopic pregnancy.
The main limitations of our study are its retrospective design, precluding the inclusion of a control group, and the relatively small sample. Large-scale, prospective control trials are needed to validate our results.
In conclusion, the present study provides evidence of the positive impact of SIS on spontaneous pregnancy, especially within the first 30 days after the procedure, and suggests considering expectant management in younger patients with a shorter duration of infertility, a higher functional ovarian reserve and a normal weight.