Introduction
Women with endometriosis have a higher rate of anxiety symptoms compared to healthy women [1]. This is due to the nature of endometriosis –a chronic gynecological disease frequently associated with chronic pelvic pain and/or infertility– which exposes women to high levels of stress and uncertainty [2]. For this reason, endometriosis is considered a disabling condition that may significantly compromise social relationships, sexuality and mental health.
As with other chronic diseases [3,4], distressed endometriosis women present an overall negative sense of female identity, with lower self-esteem and poor body image compared with non-distressed women [1]. While surgical management of women with deep endometriosis is a particularly stressful time, women are rarely assessed for psychological conditions during the consultation. Apart from a specialized consultation and the use of quality of life questionnaires including some items on mental health (SF-36, EHP30, EHP5, etc.), few parameters are available to the clinician to screen women for anxiety disorders [5,6].
Objects at the patient's bedside (e.g., photographs, stuffed animals (SA) and pillow cases brought from home) are common and can provide useful information about a patient even before the patient is interviewed [7]. However, the meaning of these objects to the patient is rarely investigated by physicians. Furthermore, while SAs are common in pediatric departments, they are rarely seen at the bedside of adult patients. SAs typically serve as transitional objects (TO) for children and adolescents [8]. Similarly, it has been suggested that they make solitude and strangeness more acceptable and provide comfort in distressing situations [9].
Therefore, the aim of this study was to compare the level of anxiety and depression of women hospitalized for endometriosis surgery with and without a TO represented by a SA.
Materials and methods
We conducted a prospective study in the department of gynecological surgery at Tenon University Hospital, Paris, France. The protocol was approved by a regional ethic committee (Groupe Nantais d’Ethique dans le Domaine de la Santé) and registered on reference 02651077. Oral consent to participate was obtained from each woman.
All the women included in the study were hospitalized for scheduled endometriosis surgery. For each woman, the following parameters were recorded: age at surgery, parity, body mass index (BMI), smoking status, previous surgery for endometriosis, surgical indications (pain and/or infertility).
Surgery for endometriosis was performed by laparoscopy. The first step of the surgery consisted in exploring the abdomino-pelvic cavity to exhaustively assess the endometriotic lesions and calculate the Revised American Society for Reproductive Medicine Classification (rASRM) [10] and the Enzian score [11]. As previously reported, the second step consisted in the removal of all endometriotic lesions with the intention of complete resection [12].
Mental health was assessed with a self-questionnaire during the hospitalization (Annex 1) using the “Hospital Anxiety and Depression Scale” (HADS) [13] that comprises two seven-item scales, HADS anxiety (HADS-A) and HADS depression (HADS-D) plus a full scale score, where respondents rate the frequency of symptoms ranging from 0 to 3 (with higher scores indicating poorer mental health). The presence or absence of an SA in the patient’s room was recorded by the medical team during the hospitalization. Data were compared between two groups; patients with an SA in the room (SA group) and patients without (non-SA group).
Statistical Analysis
All statistical analyses were performed using a commercially available software JMP v.14.0.0 software © (SAS Institute Inc., Cary, North Carolina, United-States). Quantitative variables are expressed as medians and interquartile ranges (IQR) and nominal variables in proportions. Univariate analysis was performed using the Wilcoxon test for continuous variables and the Fisher’s exact test for categorical variables. Statistical analysis was based on the Student’s t test and ANOVA test as appropriate for continuous variables, and the Chi-square test or Fisher’s exact test as appropriate for categorical variables. A p value of <0.05 was considered as statistically significant.
Results
Epidemiological characteristics of the population
Between January 2018 and January 2020, 90 patients underwent surgery for deep endometriosis and accepted to be included in the study. Among them, 30 patients (33.3%) had an SA in their room.
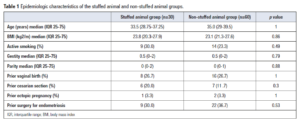
The epidemiologic characteristics of the SA and non-SA groups are summarized in Table 1. The median age was 33.5 years (IQR 28.75-37.25) in the SA group and 35 years (IQR 29-39.5) in the non-SA group (p=1). Median BMI was similar, respectively 23.8 kg/m2 (IQR 20.3-27.9) and 23.1 kg/m2 (IQR 21.3-27.6) (p=0.86).
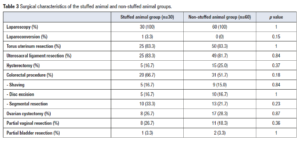
The main symptoms in the SA and non-SA groups were dysmenorrhea (100% vs 100%, p=1), dyspareunia (86.7% vs 88.3%, p=0.82), transit disorder (56.7% vs 45%, p=0.3) and dysuria (26.7% vs 18.3%, p=0.36), respectively (Table 2). Chronic pelvic pain was more frequent in the SA group (96.7% vs 70%, p=0.003). Twenty-seven percent (n=8) and 31% (n=19) had a history of infertility in the SA and non-SA groups (p=0.62), respectively (Table 2). There were no significant differences between the two groups in the rate of clinical or MRI lesions (Table 2).
Surgical characteristics of the population
The global rASRM score was higher in the SA group compared to the non-SA group; 58 (IQR 20-121.5) vs 50 (IQR 23.5-71.5) (p=0.04), respectively (Table 2). There were no significant differences between the groups for each subgroup of rASRM score: Stage I: 3.3% vs 6.7% (p=0.51); Stage II: 13.3% vs 15.0% (p=0.83); Stage III: 10% vs 18.3% (p=0.3); and Stage IV: 73.3% vs 60% (p=0.21), respectively.
A difference in the Enzian score was calculated based on intra-operative analysis (p=0.014) (Table 2). A score 3 lesion (rectovaginal space, vagina, rectal or lateral involvement more than 3 cm) was observed in 86.7% and 56.7% of patients (p=0.004) in the SA and non-SA group, respectively. A score 2 lesion (rectovaginal space, vagina, rectal or lateral involvement between 1 and 3 cm) was observed in 10.0% vs 21.7% (p=0.17) and a score 1 lesion (rectovaginal space, vagina, rectal or lateral involvement less than 1 cm) in 3.3% and 21.7% (p=0.02), of the SA and non-SA women, respectively.
All the procedures were performed by laparoscopy (Table 3). One laparo-conversion was necessary in the SA group because of extended tight adhesions (3.3% vs 0%, p=0.15). A colorectal surgical procedure was performed in 66.7% vs 51.7% of the patients in the SA and non-SA groups, respectively (p=0.18), shaving in 16.7% vs 15.0% (p= 0.84), discoid excision in 16.7% vs 16.7% (p= 1) and segmental resection in 33.3% vs 21.7%, (p=0.23) (Table 3). Eighty-three percent (n=25) of patients in the SA group and 81.7% (n=49) in the non-SA group underwent a uterosacral ligament resection (p=0.84). In the SA and non-SA groups, hysterectomy was performed in five (16.7%) and 15 cases (25.0%) (p=0.37), respectively.
Anxiety and depression symptoms and relative scores.
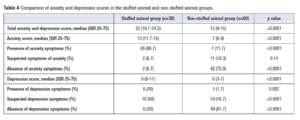
Total median anxiety and depression scores were higher in the SA than in the non-SA group: 22 (IQR 19.7-24.2) and 12 (IQR 9-15), respectively (p<0.0001) (Table 4). The median anxiety score was higher in the SA than in the non-SA group: 13 (IQR 11.7-15) vs 7 (IQR 6-9), respectively, (p<0.0001). The number of patients with a HADS-A 8+ was higher in the SA group than in the non SA group (n=28/30, 93.3% vs n=16/60, 26.7%; p<0.001). Twenty-six patients (86.7%) of the SA group reported anxiety symptoms vs 11.7% (n=7) in the non-SA group (p<0001). Seven percent of the patients (n=2) of the SA group had no symptoms of anxiety vs 70% (n=42) in the non-SA group (p<0.001) (Table 4).
The median depression score was higher in the SA group: 9 (IQR 8-11) vs 6 (3-7), respectively (p<0.0001). The number of patients with a HADS-D 8+ was superior in the SA group than in the non-SA group (n=24/30, 80.0% vs n=16/60, 27%; p<0.0001). Depression symptoms were reported by 20% (n=6) of patients in the SA group and 1.7% (n=1) in the non-SA group (p=0.002) while 20% vs 81.7% of the patients (p<0.0001) had no symptom of depression, respectively (Table 4).
Discussion
Principal findings
Patients arriving at the hospital with a SA had more severe endometriosis according to the ASRM score and described chronic pelvic pain more often than patients without a teddy bear. Most importantly, these patients were more anxious and had higher depressive scores.
Interpretation
This is in accordance with previous studies suggesting that women with endometriosis had an elevated risk of developing major depression, depressive and anxiety disorders compared to women without endometriosis [1,14,15]. Sepulcri et al. [16] showed in their study that over 80% of the women with endometriosis exhibited depressive and anxiety symptoms. Over 30% of them suffered from severe depressive symptoms and about 60% had major anxiety symptoms [16]. Cavaggioni et al. [17] reported that women with endometriosis had a higher prevalence of depressive (18.9% vs. 9.3%) and anxiety disorders (29.7% vs. 7.0%) than controls. Consistently with previous studies, Chen et al. [14] showed that women with endometriosis had an increased risk of developing major depression (hazard ratio [HR]: 1.56, 95% confidence interval [CI]:1.24–1.97), any depressive disorder (HR: 1.44, 95% CI: 1.25–1.65), and anxiety disorders (HR: 1.44, 95% CI: 1.22–1.70) in later life compared to those without endometriosis.
In our study, the risk of having an anxiety and depressive disorder was significantly higher in the SA group (p<0.0001). This is not related to the epidemiological characteristics of the population as no difference was noted between the SA and non-SA groups. Moreover, no difference in infertility was noted between the groups. This is important, as previous studies have underlined the relation between infertility and alteration in the mental score of the SF-36 questionnaire. For example, Laas et al. [18], in an international study comparing Brazilian, Italian and French populations with colorectal endometriosis, demonstrated that patients with infertility experienced an alteration of their SF-36 mental score irrespective of the country. Hence, these data imply that endometriosis should be considered and treated as a chronic disease including psychological care [19].
The role and presence of a TO in the context of a chronic disease has been widely explored in children. For example, Erkolahti et al. [8] showed that a high number of children with rheumatic disease and diabetes mellitus had a TO suggesting a delayed separation-individuation process related to the chronic disease and providing insight on coping strategies. In general populations, adolescents with a TO have been reported as having significantly more psychiatric symptoms and a poorer sense of general well-being [20,21]. Moreover, Erkolahti et al. [21] found a relation between the use of TOs and sadness in adolescents girls. As in childhood, a TO works as a defense against anxiety, especially of separation and against depression. However, it is difficult to extrapolate data from adolescents to adult women. Sparse data on the use of TO in adults in a clinical setting are available; although anecdotal reports support the belief that the use of TOs by adults in the general population is not uncommon [22].
From a clinical point of view, these data are particularly relevant. During hospitalization, the presence of an SA could be used as a tool to detect fragile patients who could be offered psychological support. Preoperatively, it has been shown that there is a relation between the MRI and the laparoscopic Enzian score [23] suggesting that patients with severe lesions are at risk of developing anxiety and depressive disorders.
As the correlation between the extent of the lesions and symptoms or pain is still under debate [24–26], our data suggest that a higher stage of the disease is associated with a higher risk of developing anxiety and depressive disorders. In a recent publication [27], the authors observed in their cohort that the age of onset of dyspareunia and infertility were both associated with the diagnosis of depression. As these two factors are associated with a more severe stage of endometriosis [25,28], they may be responsible for higher anxiety and depression HADS scores.
Limitations
Some limitations of the present study deserve to be mentioned. First, sample size of our SA group was small. However, although the exact incidence remains unknown, the overall use of SAs in the adult population would appear to be low. Second, our population was mainly composed of patients with colorectal endometriosis meaning that our data might not be transposable to patients with early rASRM stages. Third, we did not collect data on preoperative medical treatments that could alter mental health. Finally, our patients had all been referred to an expert center and had often undergone prior surgery for endometriosis thus probably representing a sub-population at high risk of depressive and anxiety symptoms.
Conclusion
Presence of a SA in the room of a patient suffering from endometriosis is a sign of vulnerability, suggesting that patients with endometriosis should be assessed for both anxiety and depressive disorders in the pre-operative setting. A rational approach to endometriosis should include an evaluation of the emotional profile to identify women who may require comprehensive psycho-somatic care. The potential benefit could be a decrease in the negative impact of surgery for endometriosis.
Declaration of interest
None