Introduction
Serum vitamin D, measured as 25-hidroxy vitamin D (25-OH-D), has traditionally been studied in diseases of the bone, such as osteoporosis [1]. However, recently 25-OH-D has been studied in pathologies nonrelated to bone disease, and hipovitaminosis D has been related to more common diseases such as arterial hypertension [2], diabetes [3], vascular disease [4] and coronary heart disease [5]. Recently, Amrein et al. [6] described in a review the worldwide status of vitamin D deficiency and stated that 40% or more of the European population had low levels, while Cui et al. [7] also described a pooled analysis of 7.9 million participants and mentioned that over 15% had some type of deficiency. Hypovitaminosis D seems to be more prevalent than previously thought, as it has also been described in French [8], Asian [9], European [10], Hungarian [11] and Italian [12] populations.
Regarding cardiovascular disease (CVD), de Boer et al. [13] carried out a 3-year prospective study that included 1,370 participants (394 with and 976 without chronic kidney disease) and was able to link low 25-OH-D levels to coronary heart disease. The lowest levels of 25-OH-D were present in patients with the highest levels of coronary artery calcifications. Kuroda et al. [14] carried out a 7-year prospective observational study in 1,232 ambulatory postmenopausal female volunteers, and was able to link low 25-OH-D levels to a higher overall risk of mortality in this population.
Carotid intima-media thickness (CIMT) measured by ultrasound has become an important noninvasive test proven to aid at stratifying patients into risk groups for CVD [15]. Nikić et al. [16] have proposed the use of CIMT to predict CVD and the risk of coronary disease. In 1994, in the Atherosclerosis Risk in Communities Study [17], that included over 15,000 patients, the CIMT was shown to have the same impact as other risk factors for CVD, and since then it has become a prospective independent risk factor for the study of CVD.
There is evidence that 25-OH-D may influence vascular function. Indeed, 25-OH-D may induce prostacyclin expression which in turn may suppress thrombotic factors, and also suppress pro-inflammatory mediators such as interleukin-6 (IL-6) and adropin [18]. Another link between 25-OH-D and vascular function may be through the matrix protein MGP, which has shown to participate in the inhibition of vascular endothelial calcifications. Braam et al. [19] have shown that low 25-OH-D levels are associated to low MGP levels, and therefore lower inhibition of vascular calcifications and thus possibly, higher risk for CVD.
Most of the previously mentioned studies were carried out in men. Nevertheless, CVD is also a leading cause of death in postmenopausal women, as it is in men. In fact, it has been shown that some women with CVD also present with hipovitaminosis D. The aim of the present study was to determine if 25-OH-D levels in postmenopausal women were correlated to CIMT, in order to propose 25-OH-D levels as an independent marker of cardiovascular risk.
Materials and methods
Subjects
Fifty-three women were screened by interview from the Hospitals’ Climacteric Clinic and according to exclusion criteria 30 otherwise healthy females were recruited. Screening was done in a consecutive non randomized fashion. All women were postmenopausal (defined by amenorrhea of at least 1 year with climacteric symptoms or history of surgical bilateral oophorectomy), and aged 45 and 65 years. Women with history of metabolic diseases that alter calcium homeostasis such as hyperparathyroidism or renal disease were excluded. Women who were consuming calcium and vitamin D supplements were also excluded. All women provided written consent, and the project was approved by the Hospitals’ Bioethical Committee, and is in accordance with Good Clinical Practice and the Helsinki Declaration II.
Samples
For investigation purposes blood samples were taken after a 08 hour overnight fast. 10 ml of blood was collected in two vacutainers with no anticoagulant. Serum was separated by 10-minute centrifugation at 1,500 g after clot formation and within 1 hour of venipuncture. All the samples were analyzed the same day they were taken.
25-OH-D was measured in serum using ELISA technique with the 25-hydroxi vitamin D enzyme immune assay by Immunodiagnostic Systems (IDS). This assay has an intra-assay variance of less than 8% and an inter-assay variance of less than 10%, sensibility of 5 nmol/L and a working range of 5 – 380 nmol/L. Total blood cholesterol and fasting glucose were also measured. After blood samples were obtained, patients were then taken to the Radiology Department where CIMT was measured. All CIMT were measured by experienced attending consultants, using a Xario Toshiba Ultrasound with a linear array transducer in B-mode adequate for this type of procedure. Both near and far wall segments of both internal carotid arteries were evaluated and the point of greatest CIMT was measured.
Statistical analysis
Statistica® software was used for analysis of data. Results are expressed as mean ± 1 standard deviation (SD). The correlation analysis between variables was performed using Pearson’s method. Comparison between groups was carried with the T Student test. For all comparisons, a p value of < 0.05 was considered as statistically significant.
Results
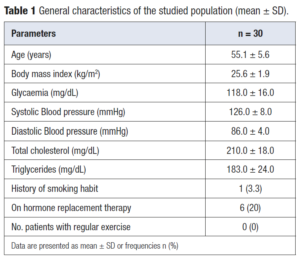
General characteristics of the study group are presented in Table 1, showing that they were otherwise healthy women in their early menopausal years.
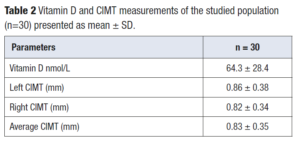
Mean 25-OH-D level of the study group (n=30) was 64.3 ± 28.4 nmol/L (Table 2). One woman presented a value of 19 nmol/L. Table 2 also shows both left and right mean CIMT values, as well as the average of both. T-student test showed no difference between left and right measurements (p=0.66). There was an isolated case were CIMT measured 2mm but was also an exception.
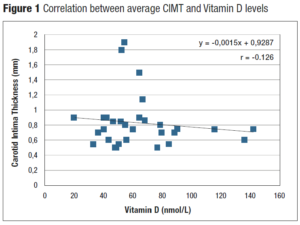
Correlation between 25-OH-D levels and CIMT was analyzed with the Pearson’s test. When the average CIMT was used, Pearson’s correlation was r = -0.126 (Figure 1). Statistical significance of dependence between these two variables was discarded due to a p=0.505. Correlation tests individually studying either left or right CIMT yielded similar results.
Discussion
The present study was based on a sample of 30 postmenopausal women with a generally good health status. Although the total number of participants was quite small, the group is very homogeneous which allows us to obtain fairly reliable results regarding this studied group. Mean 25-OH-D levels were within normal range in our group. Holick has defined hypovitaminosis as 25-OH-D levels of ≤ 20 nmol/L, and vitamin D deficiency as levels of 25-OH-D between 21 and 29 nmol/L [20]. As mentioned previously we had only one case with a 25-OH-D level compatible with hypovitaminosis, and none compatible with deficiency. Important is to consider that this study was carried out in Costa Rica, which is a country with a year-round tropical weather, where most of the population is exposed to, almost, daily sunlight. The link between geographical location and 25-OH-D levels has previously been analyzed [7-9] and has a clear physiological basis. It was expected that our population would have normal to high 25-OH-D levels, especially considering that this was an otherwise healthy population. Nevertheless, a previous study which considered a group of asthmatic patients from Costa Rica, showed that up to 85% of them had some type vitamin D deficiency [21].
In the present study, both left and right CIMT measurements were obtained in all the cases. No differences between left and right measurements were observed and validated protocols were followed [22,23] in order to have reproducible data. Both these points allow us to infer that measurements were done correctly. Gariepy et al. [24] was one of the first authors to correlate an increase of CIMT with an increase in coronary events using a CIMT threshold of 1 mm. Other authors have proposed that the threshold of CIMT and the risk for coronary events be established at 0.8 mm [25]. In our group, 8 cases (26.7%) had a CIMT greater than 0.8 mm and this aided that the mean CIMT be 0.83 ± 0.35 mm. Even though our population would not be classified as a high-risk group for cardiac events, this mean CIMT value does place them in the upper normal percentile. Related to this topic, de Boer et al. 13 and Sajjadieh et al. [26] have studied 25-OH-D levels and coronary artery calcifications, and both have been able to show an inverse relationship between these two variables. Thus, lower 25-OH-D levels predict greater coronary artery calcifications and hence, greater risk for a coronary event. Therefore, higher 25-OH-D levels are protective and associated with lower coronary artery calcifications.
We sought out to determine if a similar relationship existed between 25-OH-D levels and CIMT measurements. To our surprise, analysis revealed a very weak and non-significant inverse relationship (r= -0.126) between these two variables. If one observes Figure 1, there seems to be a tendency to propose that lower 25-OH-D levels be related to higher CIMT values. One must consider that sample size might have had an impact on results. Indeed, this was a small group (a limitation of our study); with a greater sample perhaps, a stronger correlation would had been evident and statistically significant.
Our study was not able to demonstrate a correlation between 25-OH-D levels and CIMT values. Nevertheless, our group had otherwise normal 25-OH-D levels and was not considered at high risk for coronary events. The observed tendency would have been of statistical significance if studied in a larger or high-risk group. Due to the described limitation (sample size) of our study we cannot propose 25-OH-D level measurements be used as an independent risk factor for CVD for postmenopausal women. Despite this, it is important to state that the literature has evidenced a relationship between low vitamin D levels and the increase of other markers of CVD, and that this should prompt us to study our patients for CVD each time low 25-OH-D levels are determined.