Introduction
This study was prompted by the desire of professionals on the Douala Antenatal Diagnostic staff [1] to determine, with a view to prevention, the emotional vulnerability of patients seeking procreation. Infertility is an international public health problem [2]. It is a condition characterized by the failure to establish a clinical pregnancy after 12 months of regular, unprotected sexual intercourse or due to an impairment of a person's capacity to reproduce either as an individual or with his/her partner [3]. Earlier evaluation is recommended for women over 35 who have not conceived after 6 months of attempts, and for those over 40, immediate evaluation and treatment [4,5]. There is an “infertility belt” stretching from Chad to Tanzania, including countries of the region of Central Africa [6]. Cameroon is affected and 19.2% of couples in Douala are infertile [7].
Care for infertile couples in Cameroon is part of a national healthcare system that is divided into three sub-sectors: the public sector, the private sector (comprising private non-profit health facilities such as religious denominations and for-profit facilities) and traditional medicine (Cameroon Ministry of Public Health). One out of four Cameroonians seek primary care in a health facility, and half use self-medication [8]. A study conducted in Yaoundé, Cameroon, on the attitudes and practices of women wishing to have a child found that 76% first consulted naturopaths, traditional practitioners or clerics [9]. In addition, infertility is likened to witchcraft [10]. These evidences reinforce the idea of a care pathway with heterogeneous and syncretic therapeutic itineraries that combine visits to hospitals, traditional practitioners' huts and places of worship [11], with a preference for traditional medicine. Mental health is non-existent in this healthcare panorama, extending the shortcomings observed in initial training at medical faculties in Cameroon. There are no psychologists among Cameroon's health professions.
In Douala clinics, a single attempt at assisted reproductive procreation (ART) costs an average of 3,000 euros (2 million CFA francs) and is not covered by any insurance [6]. There is a reluctance to undergo ART and to accept sperm donation [9].
Several studies have looked at the link between infertility and psychological disorders. Some hypothesized that infertility causes psychological distress. For others, psychological distress causes infertility. A third approach is concomitant psychological morbidity, on which this study is focused. A systematic review has highlighted variations in emotional distress in infertile women undergoing in-vitro fertilisation (IVF). This distress is significantly related to the success or failure of IVF [12]. Similar evidence is found in infertile men [13]. This variability of distress in the infertility context has led it being considered less as a psychological disorder and more as an emotional maladjustment in which the availability of adaptive resources is paramount [14].
Infertile patients have already developed a psychiatric disorder at the time of their first contact with a specialized fertility service and adjustment disorder with mixed anxiety and depressed mood is found in 16% of infertile women versus 4% of fertile women [15]. A 44% of infertile women show psychopathological disorders on the Symptom Check List 90 Revised, with a severity of paranoid ideation, depression and interpersonal sensitivity [16]. In Cameroon, infertility is associated with stress (84.61%) and depression (53.85%) [10]. Attitudes were dominated by anxiety (100%) and in 62% of cases, depression [9].
Psychological disorders of infertile couples are significantly associated with increasing age, higher education, longer duration of infertility and unemployment [17]. While American women with primary infertility are more distressed than those with secondary infertility [18], no significant difference was found in Malian women with primary versus secondary infertility [19]. A duration of infertility of 2-3 years has been positively associated with depression in women and those with unexplained infertility had lower depression scores than those with an identified aetiology [20]. Biological (age, primary infertility), psychological (anxiety, guilt, low self-image, A-type personality) and socio-environmental (family peer pressure, community attitude to infertility, threat of separation) factors are associated with the stress experienced by infertile couples [21]. Psychiatric comorbidity has been positively associated with the length of infertility [15]. A qualitative synthesis of evidence from infertile women in 7 African countries, including Cameroon, reported that social pressure, stigmatisation by the family and community members and financial constraints led to psychological distress [22].
In the practice of caring for infertile couples, identifying psychological distress is a feat in an environment where reproductive professionals rarely use psychologists. From a holistic perspective that includes psychological difficulties that may justify seeking a mental health professional (psychologist, psychotherapist, psychiatrist) during the various stages of the infertility care pathway, identifying couples at risk is a necessity [23].
The aim of this study was to detect psychological disorders among infertile couples and the associated biopsychosocial vulnerability factors. We posit that identifying the vulnerability factors which may affect couples in quest of procreation, would help in the development of tools and prevention strategies that would protect couples from these factors. The specific objectives were : to determine the prevalence of anxiety and mood disorders and other psychopathological decompensations of a psychotic and paranoid nature in couples; to identify the biological vulnerability factors (aetiology, type, nature, duration and treatment of infertility, history of foetal death in utero, extra uterine pregnancy, miscarriage, abortion, medical termination of pregnancy and failure of ART) and determine those associated with anxiety and mood disorders and other psychopathological decompensations of a psychotic and paranoid nature present in the couples; identify the psychological vulnerability factors (nature of beliefs, intensity of anxiety, personality trait, nature of coping strategies, nature of self-esteem, intensity of emotional maladjustment, intensity of adaptive resources, personality type) and determine those associated with anxiety and mood disorders and other psychopathological decompensations of a psychotic and paranoid nature present in the couples; identify the social-cultural vulnerability factors (age, marital status, level of education, religion, environmental pressure to become pregnant, financial difficulties and professional status) and determine those associated anxiety and mood disorders and other psychopathological decompensations of a psychotic and paranoid nature present in the couples.
Methods
Area of the study
Douala is the economic capital of Cameroon. It has around 3 million inhabitants and 6 district municipalities. Seventeen health professionals (14 gynecologists, 1 urologist and 2 general practitioners) were contacted to participate in the study and use snowball sampling. Fifteen responded favorably, for a total of 9 healthcare facilities, including 8 private and 1 public (district) hospital located in Douala I (56%), Douala III (22%) and Douala V (22%) subdivisions. In terms of technical facilities, 44% were highly performant and 56% were average. The sample was recruited from private secular (60%), faith-based (36%) and public (4%) facilities.
Period of study, study population, sampling and inclusion criteria
Data were collected from August 2015 to March 2016 (8 months). Eighty-four infertile couples, recruited through the non-random incidental sampling technique were offered a psychometric battery of tests. Thirty-four couples out of eighty-four refused to participate. Fifteen couples out of the remaining fifty were turned down as only one partner filled out the protocol’s form. Data were usable for twenty-five couples out of thirty-five and unusable for ten. We included heterosexual couples who had been trying to conceive for at least one year. As the target of our study was couples, people who did not live in the same geographical area were excluded.
Used materials and procedure
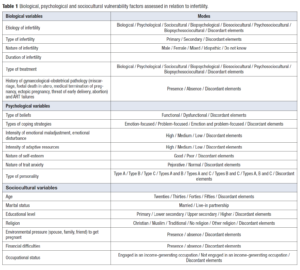
Our psychometric battery consisted of a questionnaire and 7 standardised tests. Table 1 presents the studied biopsychosocial factors and their modes. The conflicting elements express the different profiles of the couple. Are both partners involved or not?
The questionnaire included the sought biological and socio-cultural vulnerability factors, questions constructed (yes/no answers) on the basis of the diagnostic criteria for anxiety and mood disorders from Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM IV TR) [24], acute delusional disorder and items of psychotic and paranoid traits from the revised Symptom Check-list 90 (SCL 90 R). Variants of bipolar disorders were not screened. A decision algorithm was constructed on the basis of the diagnostic criteria contained in the DSM IV TR. Acute delusional disorder was validated if the person claimed that they had already had one or more periods during which they made incoherent statements, this had occurred suddenly and had lasted less than 6 months. On this occasion, she had to have ideas of grandeur or persecution associated or not with auditory, visual or cenesthetic hallucinations. She had to be totally convinced of the veracity of these ideas or of depersonalization or a constant change of mood or spatio-temporal disorientation. And finally, if these symptoms had occurred in the absence of drug use. Symptoms in the SCL 90 R were validated if the score fell within the range (0.53-1.18) for paranoid ideations and (0.3-0.9) for psychoticism.
Standardized tests were: State Trait Anxiety Inventory form Y-b (Spielberger) which assesses trait component of anxiety; Impact of Event Scale Revised by Weiss and Marmar to detect the presence of characteristic symptoms of post-traumatic stress disorder. The cut off was 33. Participants responded based on “the day/time I knew I was having trouble conceiving”. The Emotional maladjustment and Adaptive Resources questionnaire (DERA – translated and adapted from the Spanish Cuestionario de Desajuste Emocional y Recursos Adaptativos) is a screening tool for emotional imbalance and individual and interpersonal coping resources. It is used to assess the possible changes that occur at the emotional level, resulting from the need to cope with a stressful event and which do not meet the characteristics and criteria to be considered as psychopathological disorders [25]. Four subscales are differentiated: emotional maladjustment; personal resources (PR); interpersonal resources (IR) and adaptive resources (AR). The total scores obtained in each domain have been converted into percentiles which determine the position of the subject evaluated in relation to the group. There are separate scales for men and women. The scores are represented on a profile sheet used to visually determine the similarities and differences in the profiles of each partner in the couple (high, medium, low) and to identify whether or not resources are available to respond to the infertility situation. The DERA has good internal consistency with a Cronbach’s alpha of 0.85. The Dysfunctional Attitude Scale (Weissman and Burns) is used to assess the presence and intensity of dysfunctional beliefs and maladaptive thought patterns in depressed people; the Coopersmith Self-Esteem Inventory Scale to measure a person's self-assessment, the confidence in which an individual believes in his or her ability to succeed and in his or her social and personal value whatever the circumstances; and the Ways of Coping Check-list (Lazarus and Folkman) to measure the coping or adjustment strategies used when confronting a stressful situation. The protocol was completed with the “What is your personality type?” questionnaire designed on the basis of the DSM IV diagnosis criteria for personality disorders.
Data collection was adapted to the constraints of the field and to the context in which couples are treated for infertility. It was carried out by the same trainee clinical psychologist in a space made available to her or in the waiting room, except the public hospital where it was carried out by the general practitioner. The incidental sampling technique made it possible to analyze the available number of units. The couples were seen after the medical consultation, except those of the urology centre who were seen beforehand. they were contacted as part of a campaign to provide specialist infertility consultations and treatment for couples with infertility. Once informed, consent was obtained, and the couples filled out the clinical psychometry tool and the questionnaire separately. The tests were filled out on site or at home; in the second case they were returned in a sealed envelope to the medical team during the next appointment. The trainee clinical psychologist used the holistic perspective judgement to identify situations that made the questionnaire unusable. Some participants agreed to be contacted directly by her to collect the psychometric battery.
Data analysis
Using the scores of the various tests, the semiology of the DSM IV TR and the Statistical Package for the Social Sciences software (SPSS version 18.0), data was analysed to see whether or not both partners of the couple were concerned. The Cramer’s V, chi-squared and phi tests were used to determine the dependence (and its magnitude) between the biological, psychological and sociocultural vulnerability factors and the anxiety, mood, psychotic and paranoid symptoms.
Results
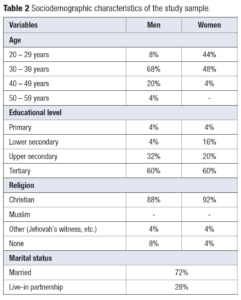
The battery of psychometric tests was usable in 25 couples. The average age of women was 29.96 ± 5.20 years and the average age of men was 36.2 ± 5.82 years. The couples were 96.4% Cameroonian. Table 2 shows the sociodemographic characteristics of the couples.
Infertility data
Infertility was primary in 52% of the cases and in almost a quarter of the cases, one of the partners had a child from a previous relationship. A 28% of couples had wanted to have children for 2 years; 32% for 3 years; 8% for 5 years; 12% for 6 years and 4% for 1, 9, 10 and 11 years. The cause was male in 47%, female in 6%, mixed in 23% and idiopathic in 6%. An 18% of the couples said they did not know who of the two was infertile. The average duration of infertility was 4.02 ± 2.63 years and 16% were undergoing assisted reproduction. A 4% had already had a failed assisted reproduction treatment. In general, the causes were oligoasthenoteratospermia (OAT) in 64%. Sexual difficulties (absence or low frequency of sexual relations, sexual dysfunctions) were mentioned by more than a quarter of respondents. Five couples were undergoing an ART protocol: two artificial inseminations with spousal sperm, two IVFs and one IVF with intracytoplasmic sperm microinjection (ICSI). Table 3 shows the characteristics of the sample based on the infertility data.
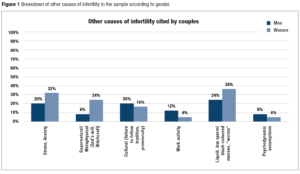
Data were self-reported by the respondents and not from the medical record. An 88% said they did not consume tobacco and in 12% there was missing information. All etiologies relating to the pathophysiology are included in the biological category. In addition to biological causes, other causes were found (Figure 1).
Psychological disorders
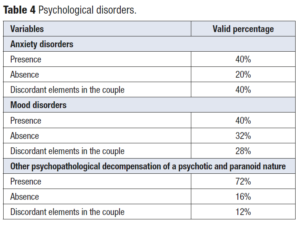
Upon analysis, it was found that in both members of the couples, 40% had anxiety disorders; 40% had mood disorders; and 72% had other psychopathological decompensation of a psychotic and paranoid nature. Moreover, one partner and not the other was affected in 40% of anxiety disorders, 28% of mood disorders and 12% of psychotic and paranoid symptoms (Table 4).
A 28.9% of the partners were traumatised by the discovery of their infertility. An 11.1% had panic disorder with agoraphobia, 8.9% panic disorder without agoraphobia, 16.2% agoraphobia without a history of panic disorder, 22% had social phobia, 14.3% a specific phobia, 23.8% obsessive-compulsive disorder, 17.8% generalized anxiety disorder and 10.3% anxiety disorder not otherwise specified. Concerning mood disorder, 36.7% had a major depressive disorder, 6.8% a dysthymic disorder, 10.4% bipolar disorder and 12.2% an unspecified depressive disorder. Regarding other psychopathological decompensation of a psychotic and paranoid nature, acute delusional disorder was detected in 2.1% of participants and psychotic and paranoid symptoms were detected in 85.7% of participants according to the SCL 90 R.
Descriptive analysis of biological, psychological and sociocultural vulnerability factors related to infertility
The etiology of infertility was biological (24%), biological and sociocultural (12%) and biopsychosocial (8%). One out of four couples (25%) used only medication, surgery and/or ART treatments. Nearly 2 out of 4 couples (45%) combined hospital visits with visits to traditional medicine huts and places of worship. No couple met with a psychologist. 4% of couples experienced in utero foetal death; 4% ectopic pregnancy; 20% miscarriage; 4% threat of early delivery; 4% abortion and 4% medical termination of pregnancy.
Beliefs were dysfunctional in over half of the couples (54%) and in one partner in 32% of the cases. A 62% had a type-A personality. Emotional maladjustment was present in 17% and in 28% it was of varying intensity depending on the partner. Although adaptive resources (AR) were of varying intensity (54%), no couple had high AR. A 39% of the couples had low self-esteem; the same was true for one of the partners (44%). A 48% of the couples combined problem-focused and emotional-focused coping strategies while a quarter (28%) only used emotion-focused coping.
A 71% of couples felt family and social pressure (family members, in-laws, spouse, friends, colleagues) to become pregnant. Furthermore, even if these couples had an income-generating activity, half faced financial difficulties that made access to care challenging.
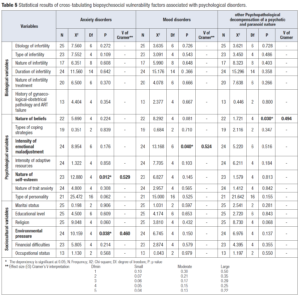
Vulnerability factors associated with psychological disorders
Specific etiology and treatment were not included in the analysis. Inferential analyses were carried out on the basis of a bio-psycho-social perspective (Table 1). The cross-tabulation of variables (Table 5) showed a statistically significant relationship between:
- Nature of self-esteem and anxiety disorder.
The chi-square test of independence performed to evaluate the relationship between these variables showed that the relationship was significant, χ2 (4, N = 23) = 12.880, p = 0.012. The magnitude of the dependency was large (Cramer’s V= 0.529).
- Environmental pressure to become pregnant and anxiety disorder.
The chi-square test showed that the relationship between these variables was significant, χ2 (4, N = 24) = 10.159, p = 0.038. The magnitude of the dependency was large (Cramer’s V= 0.460).
- Intensity of emotional maladjustment and mood disorder.
The chi-square test showed that the relationship between these variables was significant, χ2 (6, N = 24) = 13.168, p = 0.040. The magnitude of the dependency was large (Cramer’s V= 0.524).
- Nature of beliefs and other psychopathological decompensation of a psychotic and paranoid nature.
The chi-square test showed that the relationship between these variables was significant, χ2 (4, N = 22) = 1.721, p = 0.030. The magnitude of the dependency was large (Cramer’s V= 0.494).
The nature of self-esteem and environmental pressures to become pregnant appeared to be large risk indicators for anxiety disorders in infertile couples. The intensity of emotional maladjustment appears to be a large risk indicator for mood disorders and the nature of beliefs appears to be a large risk indicator for other psychopathological decompensation of a psychotic and paranoid nature.
Discussion
The aim of this study was to detect psychological disorders (anxiety disorders, mood disorders and other psychopathological decompensation of a psychotic and paranoid nature) in infertile couples and the associated biopsychosocial vulnerability factors. It was found that in 40% of couples both members had anxiety disorders, 40% had mood disorders, and 72% had other psychopathological decompensation of a psychotic and paranoid nature. Moreover, one of the two partners was affected in 40% by anxiety disorders, 28% of mood disorders and 12% of psychotic and paranoid symptoms. None of the investigated biological factors was statistically associated with psychological disorders. Concerning psychological variables, only the nature of self-esteem was statistically associated with anxiety disorders; the intensity of emotional maladjustment with mood disorders and the nature of beliefs with other psychopathological decompensation of a psychotic and paranoid nature. In relation to socio-cultural variables, only environmental pressure to become pregnant was associated with anxiety disorders. The magnitude of the dependency was large.
Presence or absence of psychological disorders
The results seem difficult to compare with those of other studies conducted on a Cameroonian population, as ours concerned couples and the gender variable was not included in the analysis. However, 36.7% of our sample had a major depressive disorder, which is lower than the rate found by Nana et al. [10] 53.85% and Ngo Um et al. [9] with 62%. This discrepancy in results may be due to the non-specification of depressive disorders in these earlier studies. It is possible that their population was affected by several types of depressive disorders. If this were the case, our results would be similar to theirs, with mood disorders present in 66.1% of the couple's partners.
Although our study concerned the couple entity, the results also seem similar to one study carried out in Iran [16] where psychiatric disorders were found in 44% of patients with an exacerbation of paranoid symptoms. Unlike a study from Teheran [17], where obsessive-compulsive disorder was the most prevalent anxiety disorder with higher score observed in infertile females than infertile males, in our study it was post-traumatic stress disorder. Although infertility is not a trauma with a capital “T” as defined by the DSM, the discovery of infertility is a challenging life event and represents a trauma as defined in Francine Shapiro’s adaptive information processing model [26]. Obsessive-compulsive disorder comes in second place here.
Biopsychosocial factors associated with psychological disorders
Unlike other studies [15,18),20,21] where a link has been found between biological factors and psychological distress, this was not the case in our study. This can probably be explained by the small sample size. Further studies with a larger sample size should be carried out. Self-esteem and environmental pressures were also found in the study carried out in Abidjan [21], although the link was with stress, whereas in our study it was with psychological disorders.
Study limitations and strengths
The used sampling technique constitutes a significant bias and the chi-square test, for small sample sizes, increases the risk to type I and II errors. Gender differences were not included in our study. Infertility data were self-reported by the respondents and not assessed from the medical record. It is possible that the studied psychological disorders and the reported sexual difficulties were present prior to the diagnosis of infertility. Unfortunately, our study cannot rule this out. The tool used to identify the presence or absence of psychological disorders is a screening tool, not a diagnostic tool. The use of structured diagnostic interviews performed by trained professionals remains recommended. All these limitations should be included in future research. We believe that including mental health professionals in the management of infertility in couples would contribute to overcome the above-mentioned limitations.
This study is a contribution that highlights the need of offering psychological (psychological assessment, etc.) and psychotherapeutic interventions to people in Cameroun whose mental health risks are no longer in doubt. It incorporates the complexity of the care pathway for infertile couples from a biopsychosocial perspective.
Conclusion
Based on the hypothesis that in the context of infertility, couples present psychological disorders whose associated vulnerability factors are biological, psychological and socio-cultural, the present study was conducted to (1) identify the presence or absence of anxiety disorders, mood disorders and other psychopathological decompensation of a psychotic and paranoid nature, (2) identify which biopsychosocial vulnerability factors are associated with these psychological disorders. The results show the presence of (1) anxiety disorders in 40% of cases in both members of the couple and in 40% of cases in one of the two partners; (2) mood disorders in 40% of cases in both members of the couple and in 28% of cases in one of the two partners; (3) other psychopathological decompensation of a psychotic and paranoid nature in 72% of cases in both members of the couple and in 12% of cases in one of the two partners. Regarding the investigated biopsychosocial vulnerability factors: (1) no biological vulnerability factors were associated with the psychological disorders present; (2) the nature of self-esteem was associated with anxiety disorders, the intensity of emotional maladjustment was associated with mood disorders and dysfunctional beliefs were associated with other psychopathological decompensation of a psychotic and paranoid nature; (3) environmental pressures to have a baby were associated with anxiety disorders. Assessing psychological variables as early as possible allows for a more serene approach in order to obtain appropriate care when trying to conceive. The value of psychological interventions for infertile patients is increasingly being documented [27,28]. Reproductive health and ART professionals in Cameroon are encouraged to seek psychological intervention for their patients. Article 20 of the Cameroonian ART Act, enacted on 14 July 2022, stipulates the need for psychological support before and during the ART process [29].